Auto logout in seconds.
Continue LogoutAlthough 64% of health systems rely on locum tenens physicians, few truly maximize their potential. Revenue loss rarely comes from using locum physicians, but rather how health systems deploy them. Used strategically, locum tenens physicians can help preserve patient access, support clinical teams and protect margins during coverage gaps. By weaving locums into long-term workforce strategy, health systems can unlock predictable coverage, reduce staffing volatility, and create scalable solutions for a future-ready physician workforce.
Forward-thinking health systems are formalizing their payer enrollment, standardizing billing operations, and strengthening clinical integration for locum providers. Instead of treating locum tenens as a temporary fix, health systems are using them to protect care access, safeguard revenue, and drive growth. Melinda Giese, SVP Enterprise Client Solutions at CHG Healthcare, outlines three actions health systems can take to unlock the value of strategic locum utilization.
1. Activate revenue opportunity from day one
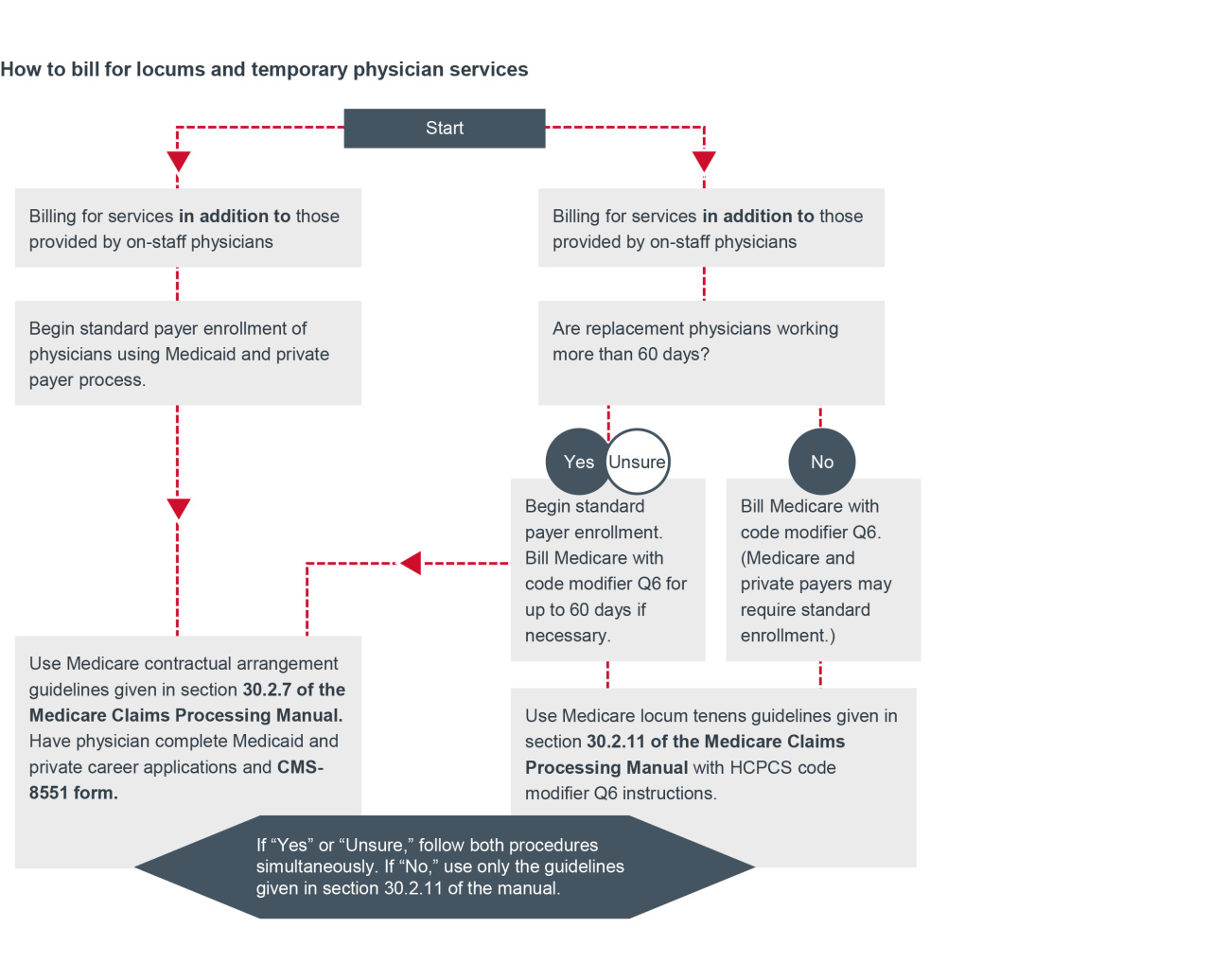
Billing for locum physicians requires proactive planning. Every locum can be billed, whether they're covering as a replacement physician, for fewer than 60 days, or serving as supplemental staff. But in many health systems, enrollment is delayed until after the physician is on site. This delay results in uncompensated or under-reimbursed care.
Future-ready health systems ensure every patient encounter is billable from the start. When enrollment is built into the deployment plan, locums can contribute to gross patient revenue from the moment they walk through the door.
|
Take several steps to avoid gaps in revenue
- Classify the physician early as "replacement" or "supplemental" to trigger the correct enrollment path.
- Start payer enrollment in parallel with credentialing — not after.
- Prioritize the three to six highest-volume payers in your market to ensure claims submissions can begin early.
- Align vendor and internal timelines to eliminate gaps.
- Leverage Q6 Modifiers and Form CMS-855I to streamline day-one reimbursement across Medicare, Medicaid, and commercial plans.
2. Plan for vacancies and keep credentialing timely
Most health systems initiate recruitment and credentialing after a physician departure is announced. Credentialing delays remain one of the most underestimated bottlenecks in healthcare staffing. Additionally, a long time-to-fill process threatens patient access, patient trust in the health system, and revenue streams.
To illustrate, a psychiatrist resigns and will leave in 60 days. A reactive health system starts sourcing a locum around day 30, and they can’t start the credentialing process until a doctor is confirmed. By the time the locum is credentialed and arrives on day 60-180, the Q6 modifier rule no longer applies. Because standard enrollment steps have been bypassed, the locum psychiatrist goes unbilled to commercial and public payers. Total gap in billing: 120 to more than 150 days, costing an estimated $768,000 in lost revenue.
In contrast, a proactive health system already has a physician staffing partner that can begin candidate outreach the same day the resignation is given. Credentialing and payer enrollment can both start. By day 60, the locum is credentialed and enrolled, patients are being seen, and claims are being submitted. Total gap in billing: 60 days or less, with no lost referrals, service line closures, or chaos.
Pre-credentialed or early-credentialed locums support seamless transitions, protecting both patient continuity and system margins.
3. Treat locums like clinical equals to catalyze workforce innovation and growth
Future-ready organizations create proactive locum tenens utilization as part of their physician workforce strategy. They use locums to launch service lines, test market demand, extend high-margin throughput, and strengthen long-term recruitment pipelines. That means locum tenens physicians are no longer just a coverage tool, but a catalyst for growth.
To make it work, treat locums like clinical equals: Integrate them into schedules, provide full systems access, and align with them to maximize coverage and productivity. Locums who are deployed with this lens become a lever for potential innovation and agility, even as systems scale.
Final thoughts
By activating revenue potential from day one, anticipating vacancies, and integrating locums as clinical equals, health systems can protect revenue and maintain patient care continuity. With proactive planning, locum tenens physicians become key contributors to growth — ensuring health systems remain agile, resilient, and ready for the future.
As the nation’s leading physician workforce experts, CHG Healthcare connects physicians, advanced practice providers, and allied health professionals with healthcare organizations nationwide - helping deliver high-quality care to more than 20 million patients every year.
With more than 40 years of experience, CHG Healthcare and its family of brands deliver scalable, people-centered workforce solutions across the clinical spectrum - from locum tenens and permanent staffing to technology and advisory services — and are recognized for industry-leading Net Promoter Scores and partnerships with half of the nation’s largest health systems.
Headquartered in Salt Lake City with offices across the country, CHG is recognized as a top workplace for its culture of care, growth, and purpose. Learn more at CHG Healthcare.
This report is sponsored by CHG Healthcare, an Advisory Board member organization. Representatives of CHG Healthcare helped select the topics and issues addressed. Advisory Board experts wrote the report, maintained final editorial approval, and conducted the underlying research independently and objectively. Advisory Board does not endorse any company, organization, product or brand mentioned herein.
To learn more, view our editorial guidelines.

This report is sponsored by CHG Healthcare. Advisory Board experts wrote the article, maintained final editorial approval, and conducted the underlying research independently and objectively.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.

