Auto logout in seconds.
Continue LogoutThe challenge
To meet growing market demand, structural heart (SH) program leaders are focused on optimizing workflows to streamline access to treatment. Traditional workup processes for aortic valve replacement (AVR) procedures leads to an average intake to treatment timeline of 42 days. Treatment delays are associated with increased mortality rates.
The organizations
Atrium Health is a 45-hospital, integrated not-for-profit health system based in Charlotte, North Carolina. Its Sanger Heart & Vascular Institute operates from two sites and is currently staffed with three interventionalists, five cardiothoracic surgeons, four advanced cardiac imagers, one APP, four nurse navigators, and two schedulers. They perform ~500-600 SH procedures annually (half of which are TAVRs).
Sarasota Memorial Hospital is an 839-bed, not-for-profit regional medical center located in Sarasota, Florida. Its valve clinic team is currently staffed with four interventional cardiologists, five cardiovascular surgeons, seven cardiac anesthesiologists, one valve clinic coordinator, one patient care rep, nurses, cath lab staff, and echo techs. They perform 300 TAVRs and 500 other SH procedures annually.
The approach
High-performing structural heart programs manage growing procedural volumes while expediting time to treatment. They do this by augmenting their patient intake process, creating streamlined care pathways, tracking and reporting patient throughput, and prioritizing patient accessibility.
The result
Implementation of these approaches has resulted in significantly shorter referral-totreatment timelines. Enhanced patient throughput also allows for programs to grow their volumes and improve patient experience and outcomes.
How Atrium and Sarasota ensure access to timely care
These organizations recognize that providing high-quality care starts before patients get to procedure day. This case study highlights four imperatives to optimize pre-procedural processes to ensure timely care and accommodate volumes despite throughput and capacity pressures.
The four imperatives
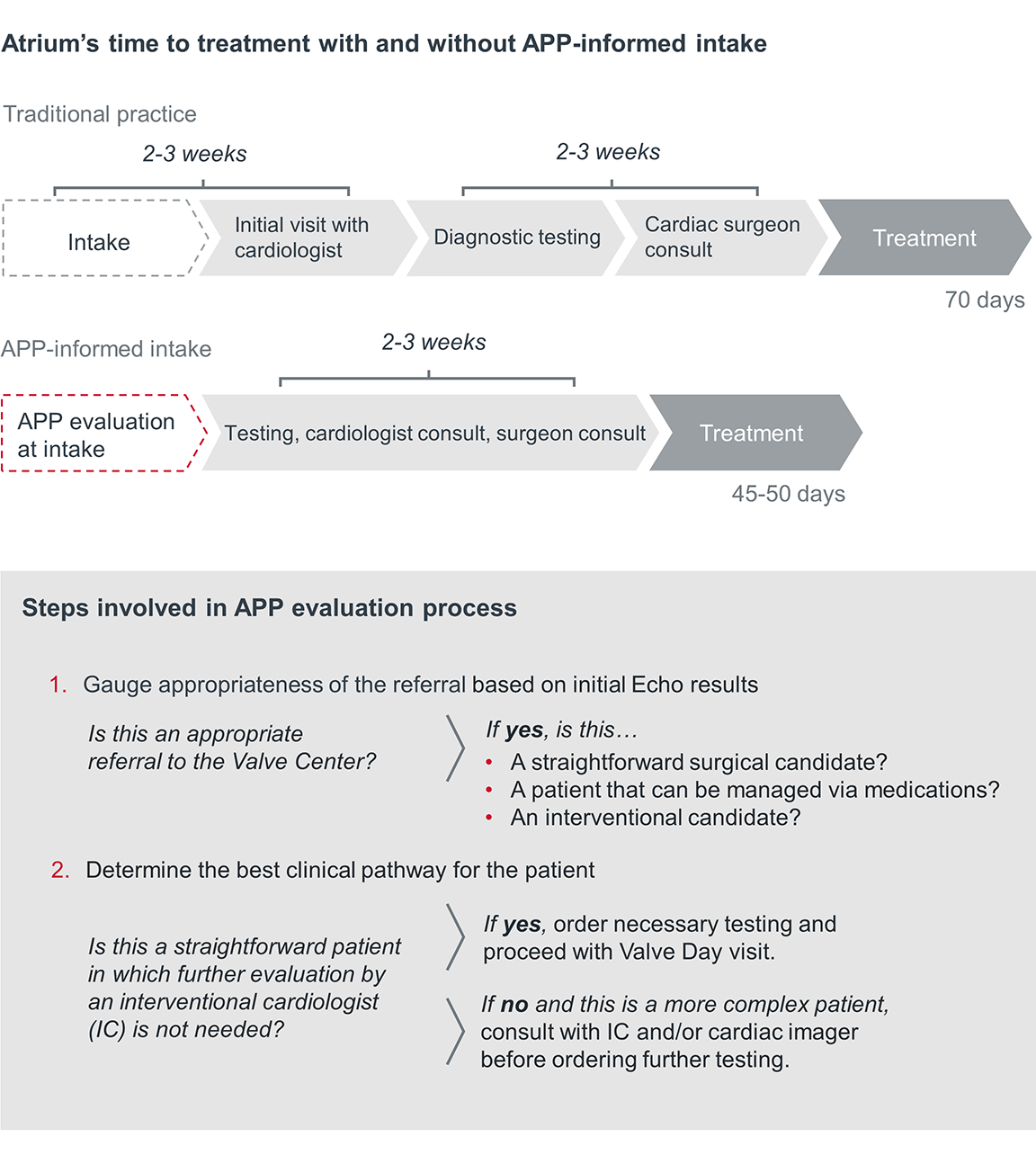
In traditional practice, a patient is referred to a structural heart program and waits up to three weeks for the initial visit with a cardiologist. Then, it takes two to three more weeks to complete the screening and physician consults needed to determine a care plan. This timeline can be further exacerbated for organizations struggling with staffing shortages or burnout, which have increased due to the COVID-19 pandemic.
Programs can expedite this process by performing an initial clinical evaluation upon referral to inform care planning. Information on a patient's disease severity, symptoms, comorbidities, and other risk factors is often available at the time of referral. Advanced practice providers (APPs) can use that information to identify diagnostic needs and schedule testing before the first physician consult. This results in a more streamlined screening process and enables earlier access to test results needed to inform treatment next steps.
How Atrium uses APPs at intake to proactively identify patient needs
Atrium encourages referral of any patient with a valve disease to their Sanger Heart & Vascular Institute. Upon referral an APP reviews existing records to perform a baseline clinical evaluation of the case. This evaluation during intake enables APPs to proactively order tests for Valve Day, avoiding long wait times prior to initiating the workup process.
Because Atrium leverages clinical input as a first step, the heart team has a preliminary understanding of the patient’s condition and can better prepare for next steps in the workup process. This pre-screening and proactive scheduling can reduce capacity constraints, minimize unnecessary testing, and enhance visibility and predictability of a patient’s care journey.
Train upskilled schedulers to operationalize early clinical evaluation
Atrium's process of APP-informed intake is possible only if all the necessary patient information is available. And that depends on the schedulers, who are the patient's first point of contact.
Structural heart programs can train scheduling staff to understand what information is needed for the APPs to make informed care decisions. These schedulers can coordinate with patients and referring physician offices to gather relevant information at intake. Upskilled schedulers are well versed in SH care and can even work with clinical staff to review previous test results, consultation notes from the referring physician, and comorbidities to risk-stratify patients and inform the patient's care plan.
Sample patient information checklist:
- Patient demographics
- Images and clinical records
- Referral notes
- Prior testing history and results
- Insurance information
Diversified treatment options and expanded eligibility for patients with heart valve diseases has led to a growing demand for care. Given that patients present with a range of conditions and severities, the number of tests and consultations needed to determine the appropriate course of treatment is time and resource intensive. It requires a multi-step pre-procedure process that relies on coordination between departments. To enhance operational efficiency and accommodate volumes, programs create standardized pre-procedure workflows with replicable steps for patient workup.
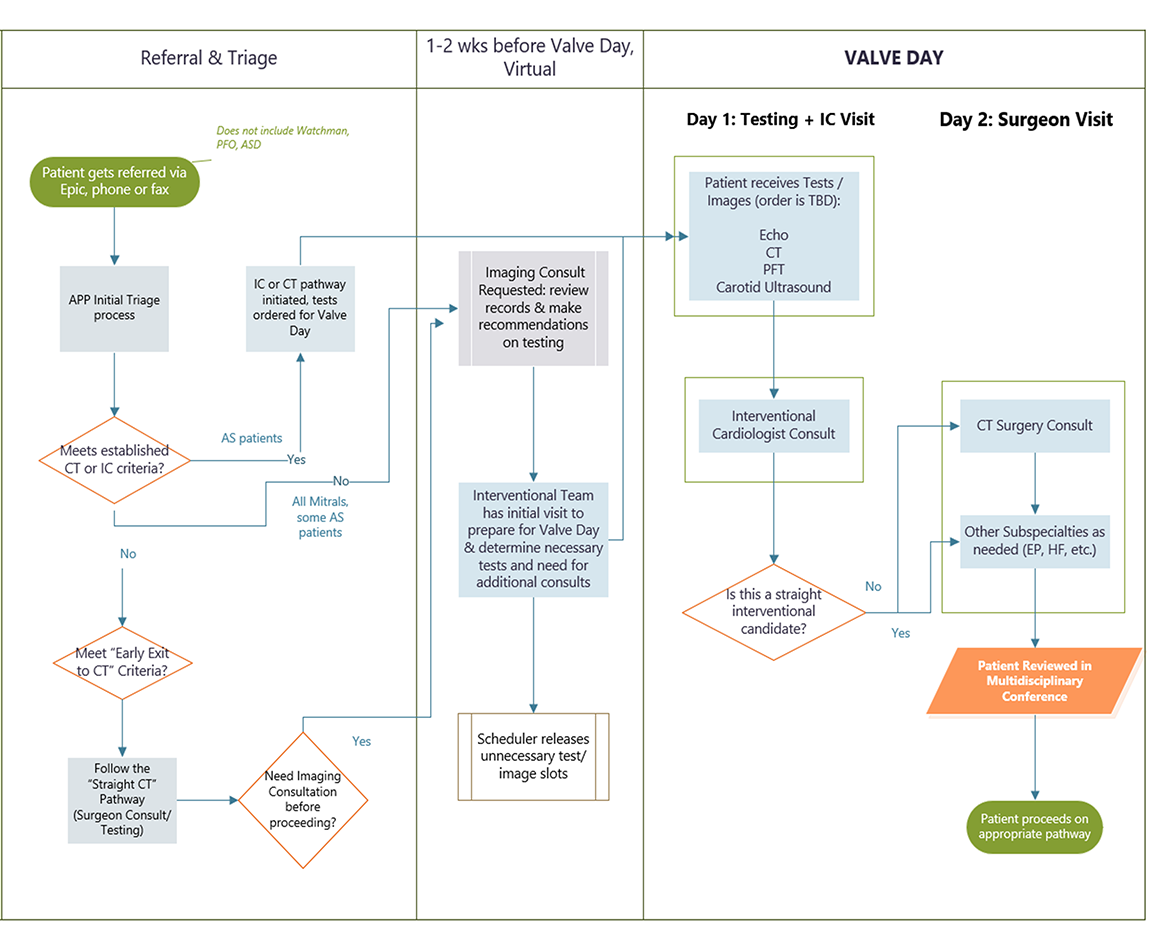
How Atrium’s standardized pathways optimize pre-procedure care
Atrium’s pre-procedure workflow (see pg. 11 of the PDF) consists of three disease-specific care pathways designed to organize patients based on workup needed prior to Valve Day. Valve Days are specific days of the week reserved for diagnostic testing and physician consults—consolidating everything into two patient visits. This process flow standardizes work to help staff anticipate workloads and allocate time and resources accordingly. As a result, patients have fewer doctor visits, and the heart team gains the predictability needed to manage growing volumes.
Elements of the optimized workflow
Condition specific care pathways
- “Fast track” patients who only need tests ordered and are ready for physician consult
- Mitral and more complex aortic stenosis patients who require additional review
- Straight surgical candidates who follow a predetermined CT surgery pathway
Consolidated Valve Days
- Day 1: Diagnostic testing & Interventional Cardiologist visit
- Day 2: CT surgery consult & consults with other subspecialties as needed
Reserved scheduling blocks
- Reserved imaging/testing access on Valve Days
- Blocks on imager calendars to create a work queue for case review
Atrium operationalizes Valve Days using reserved scheduling blocks
Valve Days are made possible by scheduling blocks that reserve access to necessary imaging and testing. Since capacity restraints can make it difficult to protect access to resources, Atrium had to make a case for why reserved access is crucial to patient outcomes and program success.
Tactics to make the case for reserved imaging and testing access
Use data to demonstrate need and potential impact
- Map out a sample patient pathway and pinpoint areas of inefficiency
- Quantify time lost to scheduling delays and highlight the timeline improvement potential of using scheduling blocks
- Compare current timelines to the 42-day national average
- Frame the ask as a patient-centered solution by explaining the correlation between care delays and adverse outcomes
Demonstrate commitment to a continued partnership
- Commit to monitoring utilization trends on a regular basis and adjust time blocks as necessary
- Guarantee to fill 8 patient imaging/testing appointment slots per week and release any slots that are not filled 72 hours in advance
By demonstrating the mutual benefits of collaboration, Atrium’s heart team was able to establish leadership-buy in and secure reserved access to weekly imaging blocks.
Atrium created an imager queue to enable access to real-time consultation
The heart team uses schedule blocks to hold time for cardiac imagers on Valve Days. They have a work queue in the EMR where imagers review and leave input during these blocks. The queue creates on-demand access to imager review, enabling the heart team to make timely, informed decisions. Many organizations wait until the next multidisciplinary conference to get input from imagers, creating unnecessary delays.
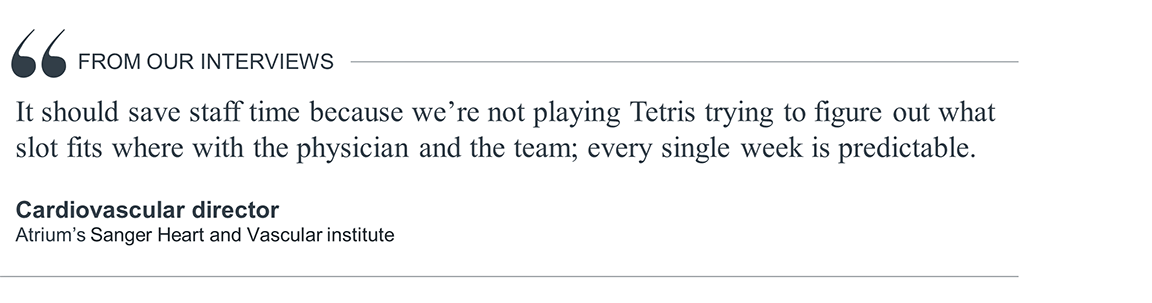
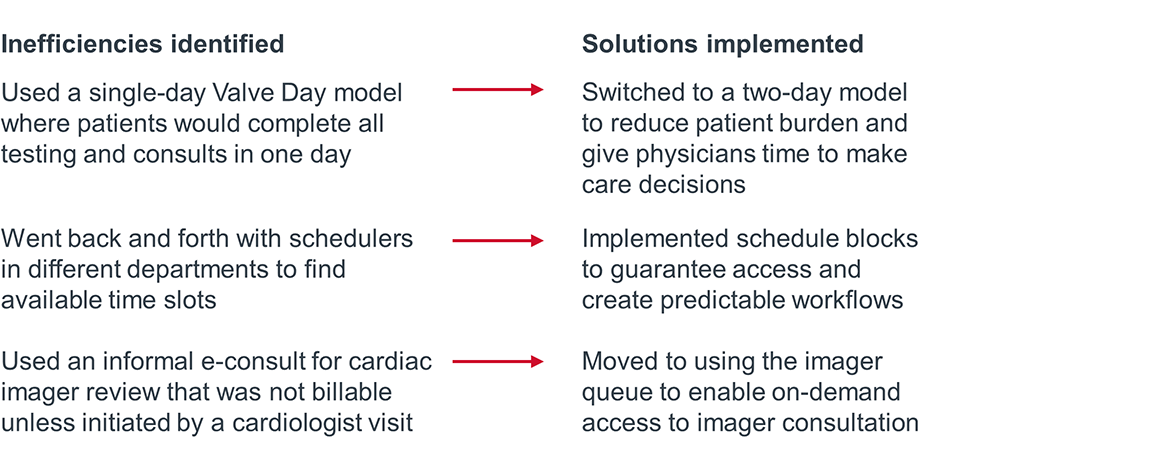
How Atrium continues to adjust processes to enhance efficiency
This work requires trial and adjustment. Programs should continually evaluate and adapt their processes to identify areas for improvement, increase workforce capacity, and continue to meet growing volumes.
Since creating their valve center process flow in August 2021, Atrium has identified areas for improvement and implemented new solutions.
Atrium Health’s Sanger Heart & Vascular Institute’s Valve Center Process Flow
Atrium Health’s Sanger Heart & Vascular Institute developed the below process flow to optimize pre-procedure patient workup.
Programs can better manage patient volumes and reduce unnecessary wait times by aligning heart team members on their goals. Establishing reliable tracking methods and deliberate communication channels ensures everyone is on the same page, helping the patient to efficiently progress through the workup process and receive timely treatment.
Sarasota tracks active cases to ensure patients progress to treatment accordingly
The Valve Clinic Coordinator (VCC) maintains two systems to track all active cases, update patients position in the care pathway, and prioritize patients based on their health status or urgent needs.
1. List of all patients
- Updated 2-3 times a day
- Documents patient information/preferences that would be pertinent to a performing physician
- Lists assigned staff members
2. Calendar that shows where each patient sits in the care pathway Shows all active cases
- Color coded by physician
- Provides a visual aid to quickly see each physician's case load
Paying close attention to where each patient is in the workup process ensures patients receive treatment within the target timeframe. Case by case tracking helps individualize care by keeping patient names and their treatment plans highly visible.
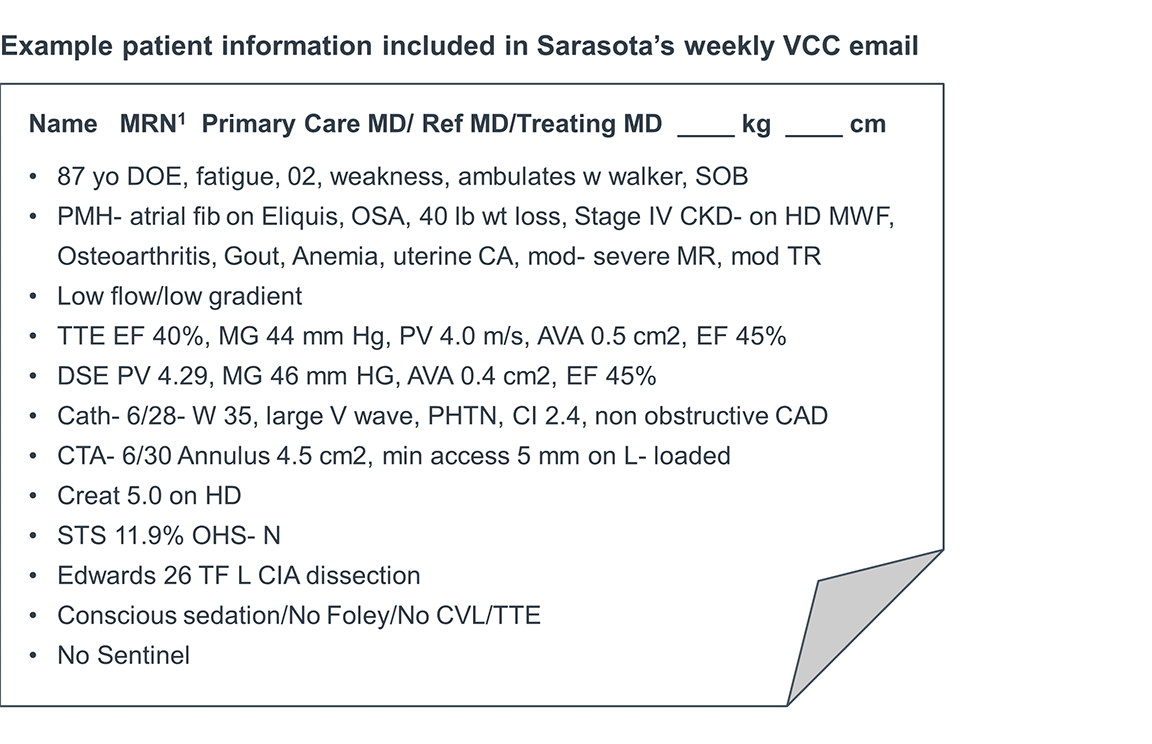
Sarasota’s VCC distributes a weekly email to enhance alignment and accountability
The weekly email serves as an at-a-glance resource to inform team members about upcoming procedures and schedules. Enabling immediate access to patient information fosters team alignment and encourages self-service rather than relying on the VCC to be the sole source of information.
Team members report knowing what to expect and where to quickly find what they need. This reduces time wasted searching elsewhere for information, gets ahead of hurdles that may prevent patients from moving through the care pathway, and helps Sarasota to reach its 14–21-day time to treatment target.
VCC weekly email includes:
- Procedure schedule including procedure approach, vendor, and device size for each patient
- Heart team and screening schedules and action items for upcoming procedures and screening
- Integrated documents and templates to support pre- and post-op processes
- An H&P template incorporating all items for ACC/TVT database collection
- Order sets for pre-TAVR and post-TAVR
- Documentation template for billing and coding
- Printed educational materials given to patients
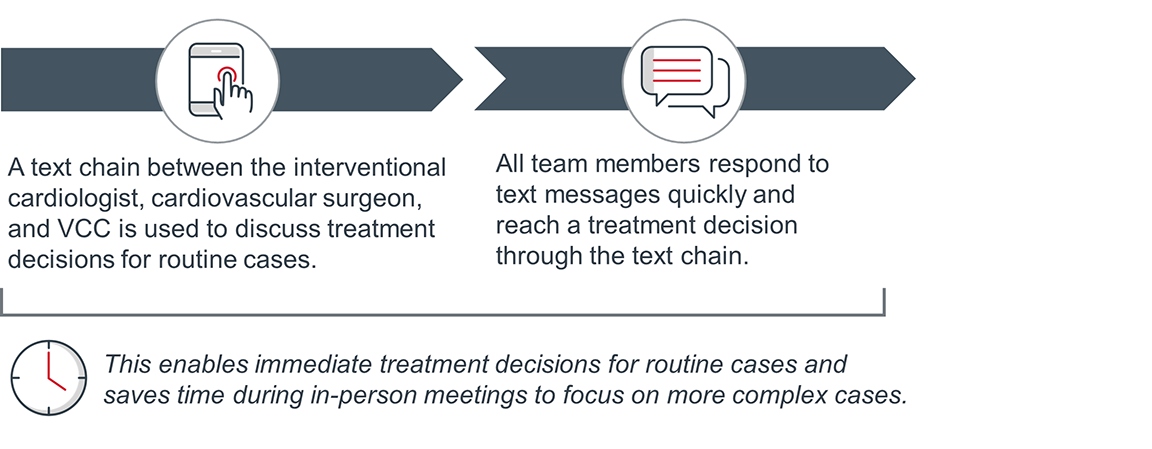
Sarasota heart team’s text message-based consultation
All structural heart programs have some form of a multidisciplinary conference to review and collaborate on cases. At Sarasota, these meetings are bi-weekly, meaning that treatment decisions could be delayed by over a week depending on timing. To make sure this bi-weekly schedule doesn’t delay treatment, Sarasota implemented a text-based consultation approach to collect real-time input from multidisciplinary team members.
How it works:

Hitting time to treatment targets is contingent on a patient's ability to navigate the many steps between referral and treatment. Programs should employ tactics to facilitate timely treatment based on common patient barriers.
Potential barriers to timely treatment
- Long distance to screening facilities
- Unreliable transportation
- Lack of pre-visit preparation
- Unanswered questions about treatment options
- Patient hesitancy to pursue treatment
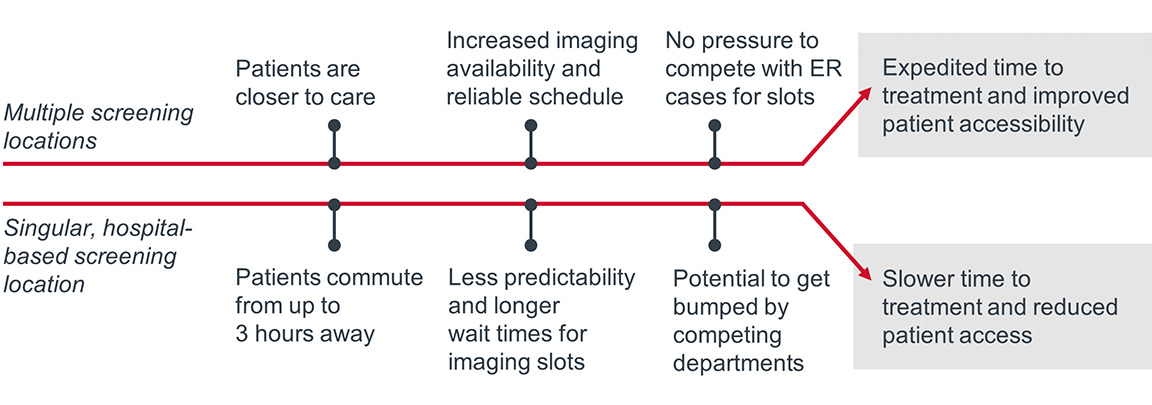
Sarasota’s screening location flexibility improves access
Sarasota utilizes multiple screening locations to increase scheduling flexibility and accommodate patient commutes. Offsite screening locations often have more availability because they’re not competing with other, high priority departments. The heart team’s access to the CT schedule allows them to prioritize urgent cases by slotting patients into the next openings.
Atrium’s patient resources enhance care quality and efficiency
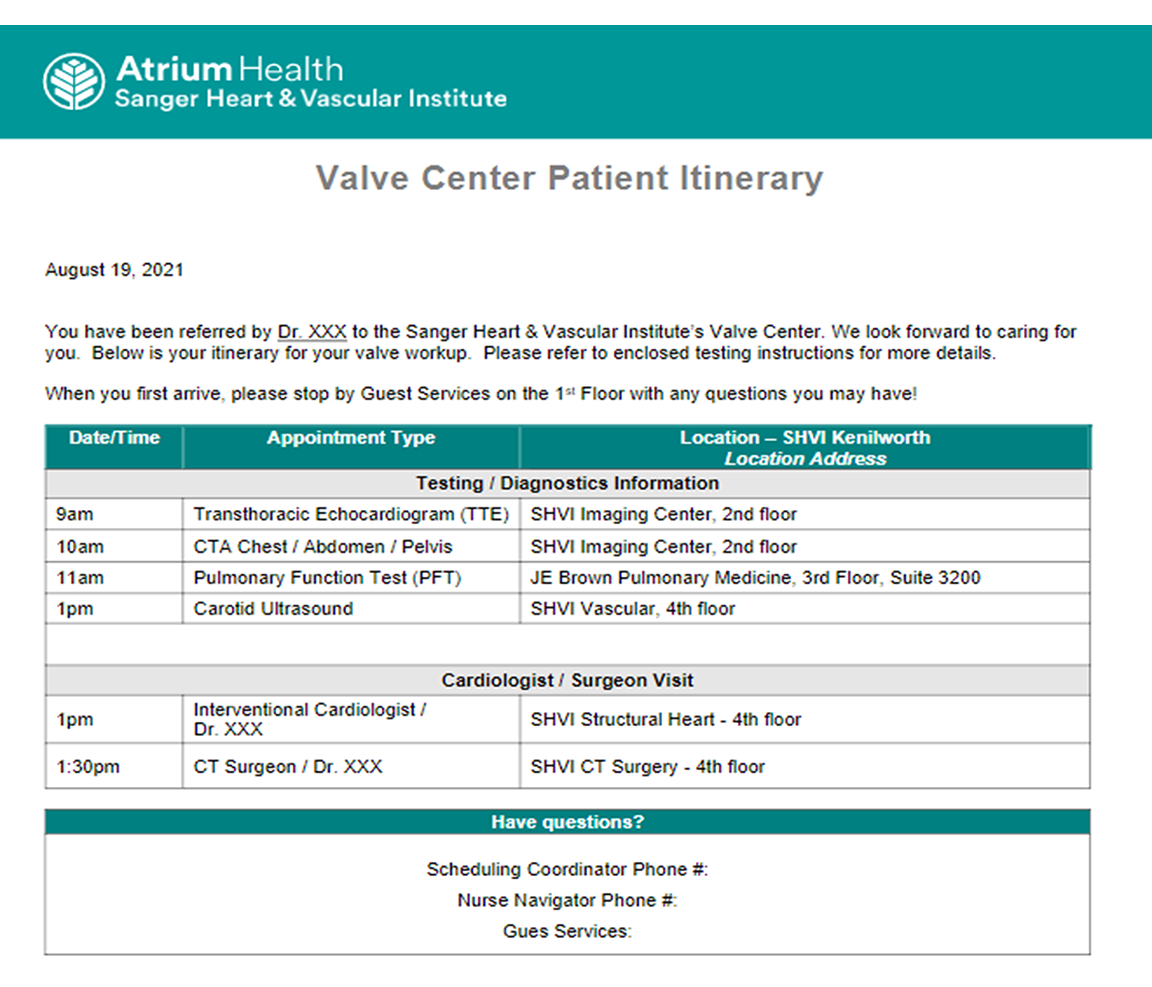
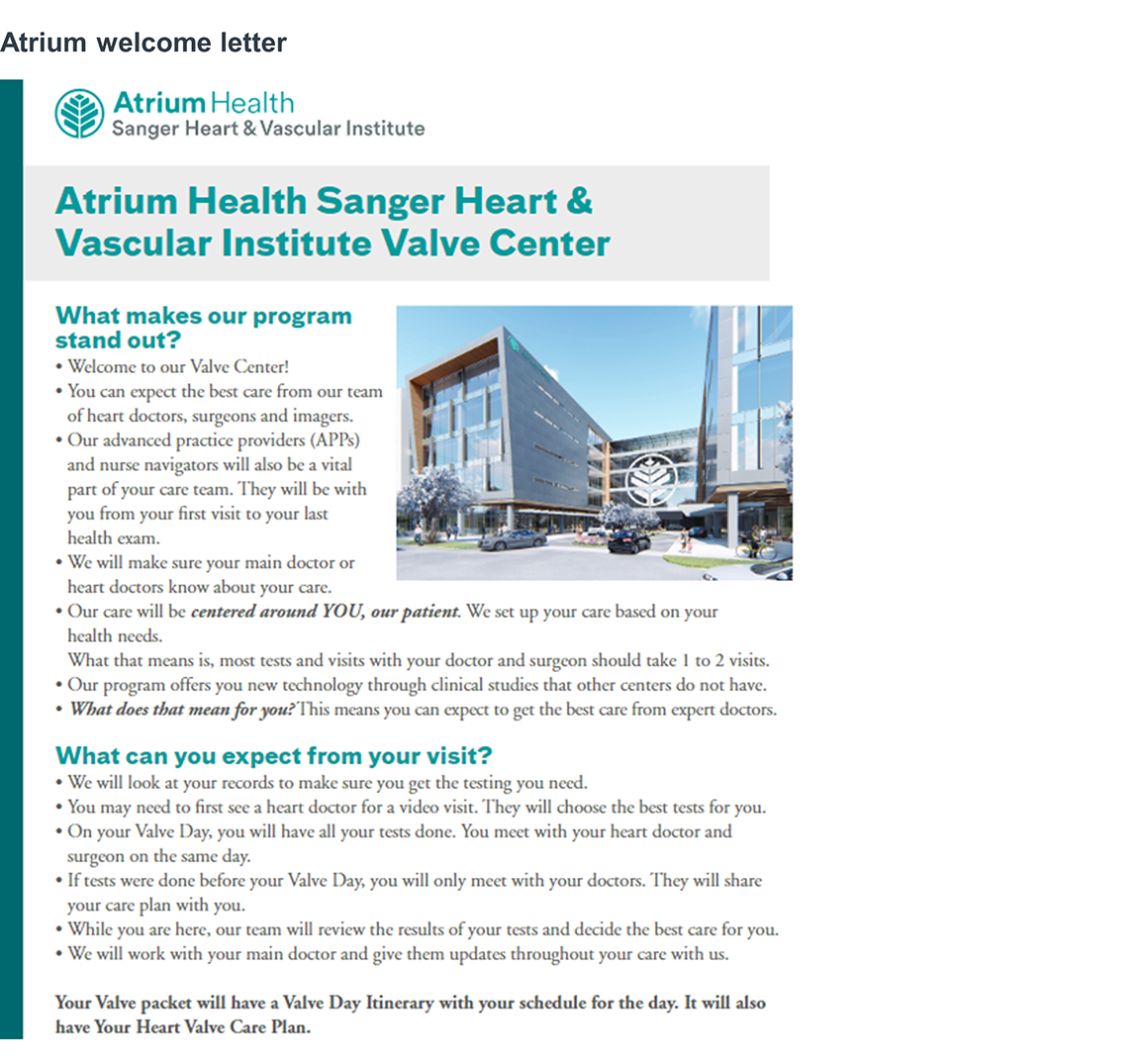
The team at Atrium recognized that the extensive workup process for SH care can be overwhelming for patients. To alleviate some of that stress and help patients navigate their care, Atrium compiled a patient resource packet to give patients a “map” of what to expect in advance of Valve Day.
Providing educational and decision aid resources in advance of in-person visits saves time on Valve Day by helping patients to develop a baseline understanding of their condition and treatment options. Access to this information helps patients feel more prepared to engage in care decisions and provides the opportunity to identify questions prior to meeting with the heart team. Programs also have the opportunity to answer patient questions outside of visits by offering immediate access to staff. One way is to leverage upskilled schedulers (pg. 7 of the PDF) who are equipped to speak to the process at a high level.
Patient resource packet includes:
- Welcome letter: to orient the patient to the program
- Valve day itinerary: includes doctor names (referring physician, SH IC, and surgeon), agenda outlining time and location for tests/consults, and contact information for patient questions
- Educational resources: an explanation of valve disease (using easy to understand language and diagrams), list and definitions of diagnostic tests, explanation of treatment options, next steps for what the patient should expect during their visit
- A decision aid for shared decision making: to facilitate patient involvement in treatment decisions and ensure they receive treatment that is the best fit
Atrium Health Sanger Heart and Vascular Institute patient itinerary
Atrium Health’s Sanger Heart and Vascular Institute uses the below patient itinerary to give patients an understanding of what to expect prior to Valve Day.
How we know it’s working
Operationalizing these imperatives has demonstrated benefits in the three key areas:
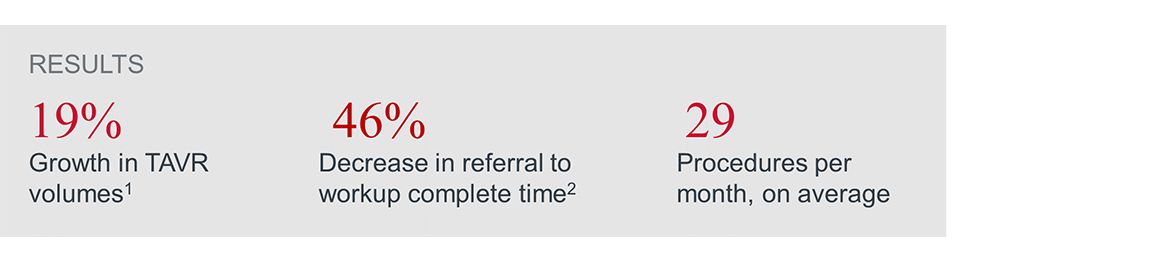
1. Appropriate and timely access to treatment: Reducing the time it takes for patients to receive an AVR procedure is essential to ensure the best possible outcomes. Sarasota was able to cut the national average intake to treatment time in half, while Atrium reduced its intake to treatment time by 25 days.
- National average: 42 days
- Atrium: 45-50 days
- Sarasota: 14-21 days
2. Growth in program capacity: Improving patient throughput allows programs to accommodate higher patient volumes. Standard care pathways help organizations identify and address inconsistences to relieve capacity constraints. Sarasota Memorial Hospital and Atrium Health both have annual TAVR volumes higher than the national average, made possible in part by their optimized workflows.
- National average: 84 TAVR procedures annually
- Sarasota and Atrium average: 250-300 TAVR procedures annually
3. Enhanced patient experience: Streamlining the pre-procedure process reduces the patient burden by limiting time spent attending doctor visits and gets them on the road to recovery sooner. Patients also know what to expect in their care, which supports a better experience.
Atrium welcome letter
Atrium’s welcome letter includes a page to orient patients to the program and set expectations for their visit (included below), and a page that includes photos and job titles to introduce the members of their heart team.
Edwards Lifesciences is the global leader in patient-focused medical innovations for structural heart disease, as well as critical care and surgical monitoring. Driven by a passion to help patients, the company collaborates with the world’s leading clinicians and researchers to address unmet healthcare needs, working to improve patient outcomes and enhance lives.
This report is sponsored by Edwards Lifesciences, an Advisory Board member organization. Representatives of Edwards Lifesciences helped select the topics and issues addressed. Advisory Board experts wrote the report, maintained final editorial approval, and conducted the underlying research independently and objectively. Advisory Board does not endorse any company, organization, product or brand mentioned herein.
To learn more, view our editorial guidelines.

This report is sponsored by Edwards Lifesciences. Advisory Board experts wrote the report, maintained final editorial approval, and conducted the underlying research independently and objectively.
Learn moreDon't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.

