Auto logout in seconds.
Continue LogoutDo you know what your members want most from you?
We asked nearly 5,000 consumers across the country which services would provide them the most value in staying healthy—and who they want these services from.
Among the top ten services members most want, members say they want their plan to be the one to help them choose the best insurance product, help them choose doctors, and help negotiate prices for medical services.
Surprised? You shouldn’t be, because it’s what you already do.
Here’s the catch—you’re not getting credit
Infographic: We took key pieces of data from this survey and outlined them in this complimentary infographic. Learn more about what consumers want when it comes to how they consume health care
All plans would say that they certainly negotiate on behalf of their consumers. But most consumers reported not having access to help negotiating prices for medical services, as shown in the graph below:
Services members want from their plans
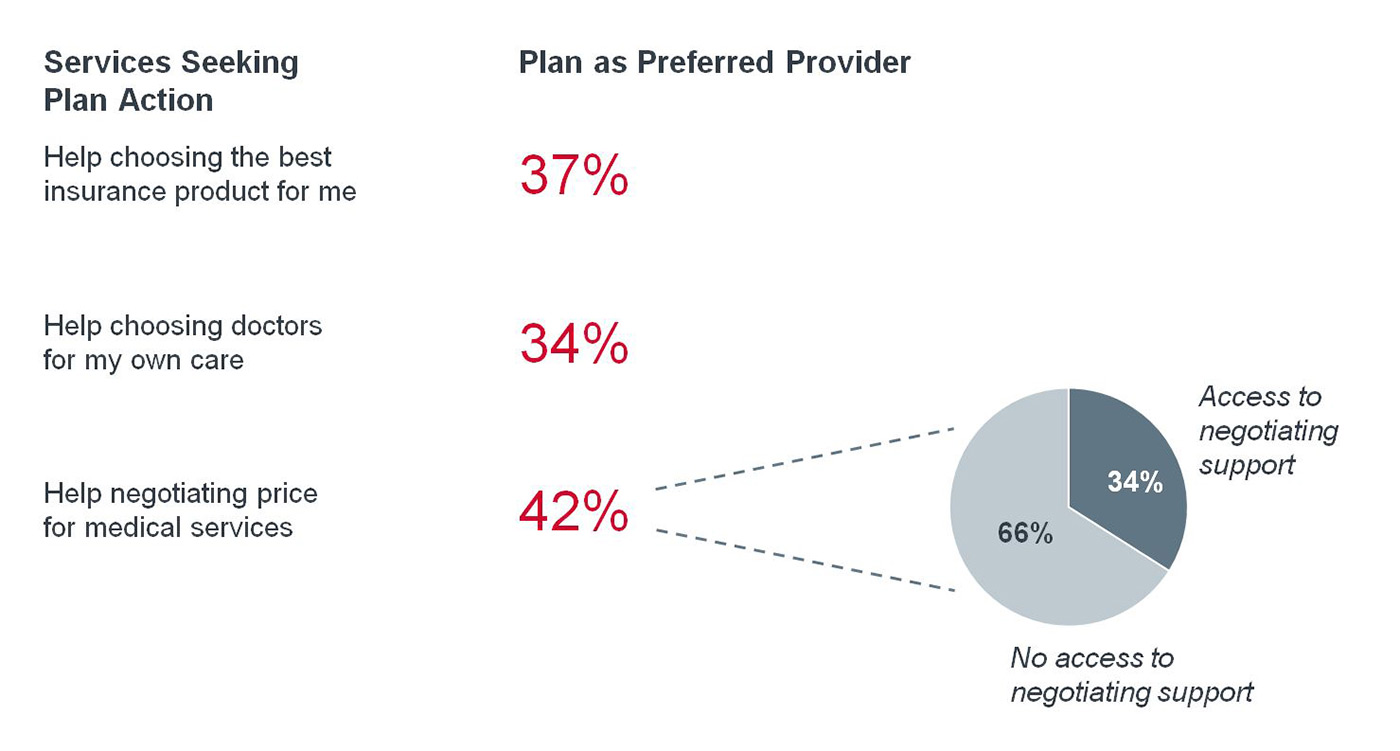
People don’t think they have access to the very service that plans offer. It’s clear that members don’t notice—or understand—the role of their plan. You are not getting credit for the work that you do.
So how can you better communicate your value to your members?
Research Briefing
Do you know how many people like their health plan? Check out this quick blog post that briefly reviews some interesting statisticsChange the way you say hello
To start, you can improve how you say hello to new members.
Plans typically bombard members with papers and emails—EOBs, call center numbers, HRAs, legal documents—and they often go in the trash. Like many plans, Anthem previously sent multiple disjointed, confusing mailings to new members—and often lost their engagement with members from the very beginning.
Anthem changed how they introduce themselves to their new members. Now, they send a personalized welcome box that combines multiple mailings into a single, simple, attractive package.
Inside Anthem's Member Welcome Box
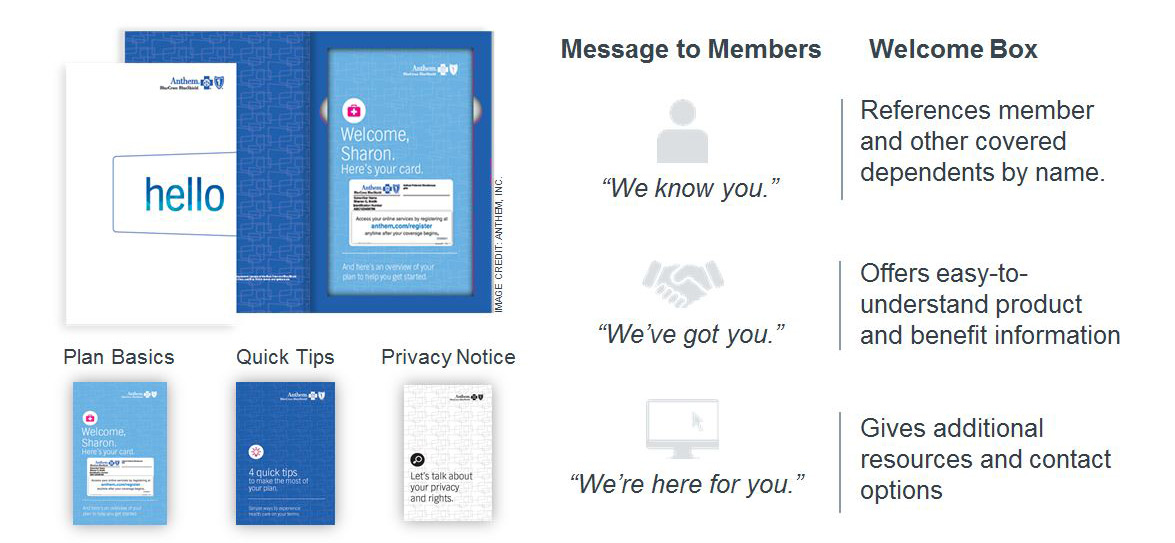
It gives members resources to understand their new plan, and clear instructions for how to contact the plan if needed—without overwhelming them.
They’ve seen a roughly 20% increase in the number of members who understand their product. These members are able to use their benefits more wisely, and contact the plan when they need help.
Personalize your interactions
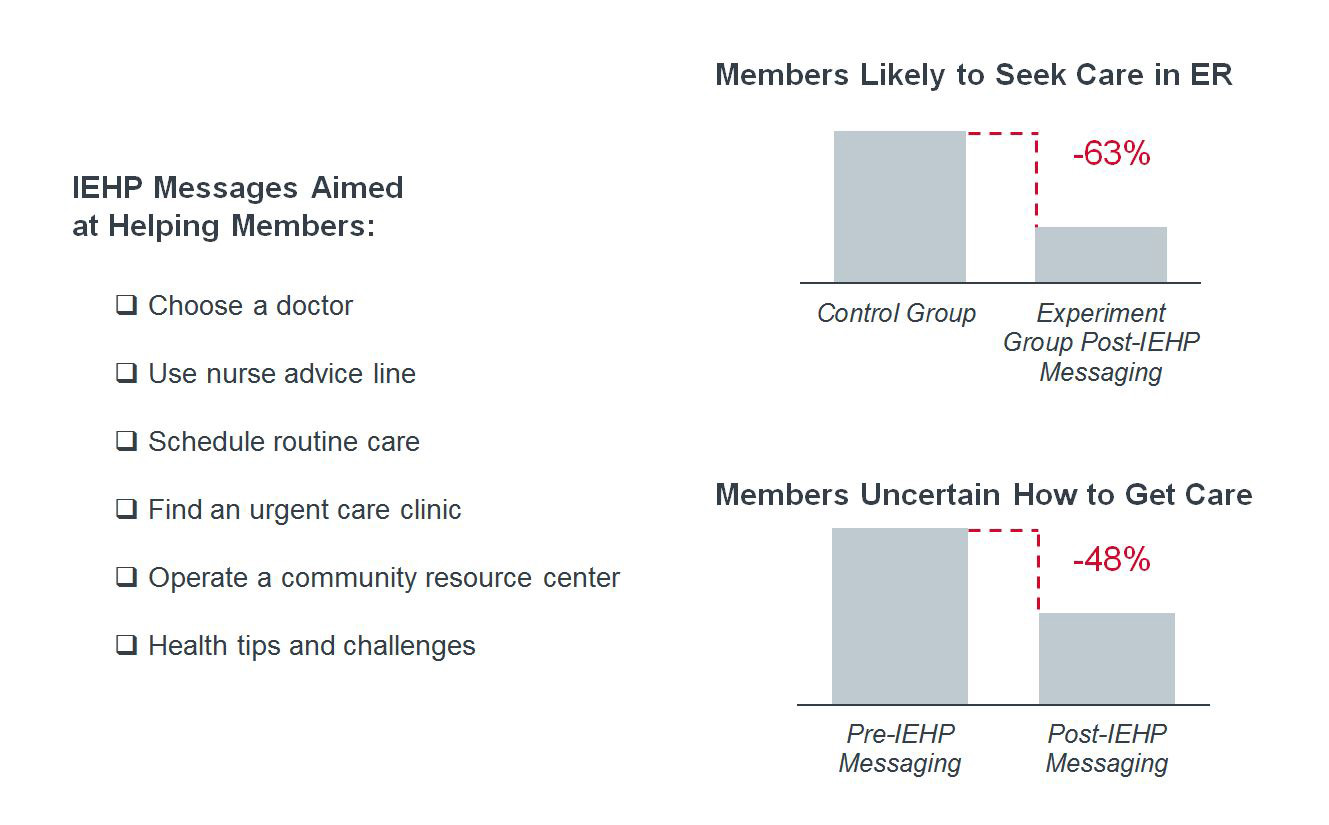
But plans also need to show their support for members, along every step of the care pathway. Inland Empire Health Plan (IEHP) partnered with mPulse mobile, a secure texting communication system, to help their Medicaid members choose a doctor, schedule routine care, and find an urgent care clinic.
They developed insight-driven messaging workflows to deliver relevant, targeted messages to members—personalized for their needs. In addition to standard demographic data, the platform also incorporates members’ conditions and personal information to target messaging.
The system can even respond to non-standard phrases like “yup” (rather than just “yes”), so the member doesn’t get a robotic “I don’t understand what you mean” response.
With this tailored communication, these members are less likely to be in the ER or be confused about how to get care. You can see outcomes from the program in the graph below:
Results of IEHP’s Mobile Messaging Program
Percentage change in members reporting selected behavior
n=17,000 Newly-enrolled IEHP members, evaluated over a three month period
About the survey:
We asked 4,879 consumers across the nation to rank health care services using MaxDiff methodology. Unlike many other surveys, which allow respondents to rate all items as “important”, the MaxDiff conjoint methodology asks participants to make trade-offs, providing insight into the relative importance of each attribute.
Respondents were shown multiple sets of healthcare services. Within each set, they were asked to choose the one “most appealing” and the one “least appealing” to them. Each attribute was presented multiple times, resulting in a ranked list of utility scores indicating the relative value of each attribute.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.

