Auto logout in seconds.
Continue LogoutThe human papillomavirus (HPV) test is able to detect precancerous changes within the cervix quicker and with more accuracy than a Pap smear, according to a new study published in JAMA—leading some to call for the elimination of the Pap smear altogether.
Get ready-to-use slides on women's health market trends for 2018
About HPV
HPV is the most common sexually transmitted infection in the United States. According to CDC, about 80 million U.S. residents are infected with HPV each year, though most never develop any health problems from the virus, because the immune system typically clears HPV infections on its own within a year or two. However, if an infection persists, it can cause cervical and other cancer. According to the American Cancer Society, roughly 4,200 women will die of cervical cancer in 2018.
According to the Washington Post's "To Your Health," most medical groups recommend that women ages 30 to 65 be co-tested with the HPV test and a Pap smear every five years. However, some experts have argued that the Pap smear test should be eliminated entirely.
Diane Harper, a professor of medicine and HPV researcher at the University of Michigan, said the Pap smear test can result in false positives, which she said affect about 30% of people, and is one of the reasons some experts have recommended doing away with the test. A false positive on a Pap smear could lead to a woman having an unnecessary biopsy during a colposcopy, which comes with risks like infections and pelvic pain, according to the Mayo Clinic.
Study details
For the study, researchers placed about 19,000 women into two groups—one using the HPV test to screen for cervical cancer and one using a type of Pap test called liquid-based cytology. The researchers screened the women using either the HPV test or the Pap test at the beginning of the four-year period. Those who received the HPV test and whose test results were negative for signs of cervical cancer were screened again at 48 months, while those who received the Pap test and whose test results were negative for signs of cervical cancer were screened again at both 24 months and 48 months. Each of the groups received both the HPV and Pap test at a 48-month exit screening.
The researchers found that there were noticeably more cases of precancerous lesions detected early among the women who received the HPV test than among those who received the Pap test. The researchers also found that there were fewer cases of pre-cancer in the HPV test group than the Pap test group.

Learn about the latest clinical innovations in oncology
In addition, the researchers found that adding the HPV test to the Pap smear group at the end of the four-year period resulted in 25 lesions found that would not have been discovered with the Pap smear alone. Adding the Pap smear to the HPV test group at the end of the four-year period resulted in an additional three lesions found that would have been undiscovered with just the HPV test, the researchers found.
Gina Ogilvie, the study's lead author and a professor of medicine at the University of British Columbia, said the findings show "[t]he real benefit of co-testing is with the HPV test," rather than the Pap smear.
Discussion
Many experts praised the study's results, saying it showed that Pap smears were unnecessary. Kathleen Schmeler, a gynecological oncologist at MD Anderson Cancer Center who was not involved in the study, said the results show "that you could potentially do just the HPV test and move toward getting rid of the Pap test."
Similarly, Mark Schiffman of the National Cancer Institute said the study confirmed the importance of moving away from the Pap smear and to the HPV test alone. Schiffman said the Pap smear is "crude and inaccurate," while the HPV test is more precise.
Jason Wright, a gynecologic oncologist at NewYork-Presbyterian/Columbia University Medical Center, said the United States Preventive Services Task Force, which currently recommends co-testing, could issue a final recommendation against co-testing in light of the new study.
However, Mark Spitzer, a gynecologist and former president of the American Society for Colposcopy and Cervical Pathology, disagreed, saying the three additional lesions found by adding the Pap smear to the HPV test group in the study justified co-testing. "In the U.S., co-testing is currently the recommended gold standard, and neither doctors nor their patients should be willing to give up the added benefit you get from screening with a Pap test and HPV test together," he said (McGinley, "To Your Health," Washington Post, 7/3; Watson, "Shots," NPR, 7/3; Ogilvie et al., JAMA, 7/3).
What they value: 5 types of cancer patients
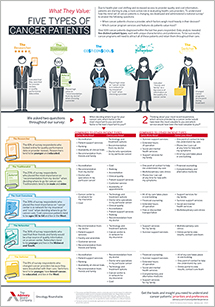
Cancer patients have more choices for their care than ever before. To attract patients in this fiercely competitive landscape, you must invest your limited resources in the right services—ones that will earn patients' trust and improve their experience.
Our infographic is your guide to understanding the five types of patients and what they value in a cancer provider.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
