Auto logout in seconds.
Continue LogoutGiven regulatory pressures and incentives, hospitals are forming narrow networks with the highest-quality post-acute care (PAC) providers to maximize the number of patients treated by top-quality providers. The problem: health systems typically struggle to develop and run these networks successfully. As health systems’ post-discharge accountability increases, the need for a high-performing post-acute network to support system goals also increases.
Below, we outline how to identify specialist PAC partners that complement your health system’s areas of expertise. We also review a case study on how TriHealth launched an initiative to address the post-acute needs of their orthopedic patients, and the variables they used to identify 13 select partners from a population of over 100.
To learn more strategies about how to optimize your post-acute network, download our guide: 10 Keys to an Efficient Post-Acute Episode – Part 2: Achieve effective patient management post discharge.
Infographic: We surveyed nearly 4,000 consumers about their care preferences and outlined the top four things post-acute patients and families want from their health care experience
An effective post-acute network must be able to care for the full range of patient types the health system serves. As such, once systems have identified providers capable of caring for their most common patient types, the network should expand to include providers with complementary expertise. Such providers may include sectors with defined admissions criteria (IRF, LTACH, and hospice), providers strong in particular specializations (e.g., traumatic brain injury), or provider types supporting high-risk areas (e.g., pharmacy).
When assessing candidates for closer post-discharge partnerships, hospitals should inform all providers in the market of the initiative and request relevant information from them to determine partnership viability. This can be done via a request for proposal (RFP). In addition to the RFP, health systems should also gather data on top providers through additional means—for example, through conducting in-person interviews or tours—rather than rely solely on the RFP to make decisions.
Implementation Advice from our Experts
- Assess hospital-specific data to determine areas for specialty alignment, including diagnosis-specific payment programs and patient volumes
- Collect data to evaluate partnership viability for the specific service line or capability in question
- Involve hospital staff (e.g., service line leaders) for the specific service line in the selection process
Case Study: How TriHealth launched an initiative to cover their orthopedic patients
TriHealth, a two-hospital system in Ohio, launched an initiative to select orthopedic Skilled Nursing Facilities (SNF) partners, given high volumes in its orthopedic service line.
To select preferred SNF partners, TriHealth analyzed the performance of each SNF receiving TriHealth joint replacement patients in the last year, collecting data and eliminating SNFs that did not meet minimum quality standards. An internal team with representatives from the service line (e.g., Program Director of Orthopedics) then conducted tours of remaining SNF facilities and completed evaluations.
Ultimately, the team selected 13 orthopedic partners, down from over 100, who now receive 88% of discharges.
TriHealth's SNF Selection Process for Orthopedic Service Line
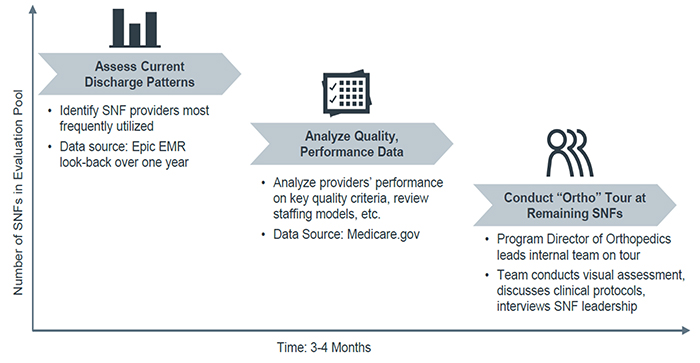
TriHealth's Initial Review Process
- Geography*: Four-county area including Hamilton, Butler, Warren, Clermont
- Attending TriHealth Physician: Physician with TriHealth Privileges
- Gather and Analyze Initial reports: Analyze report of all patients which have been referred to SNFs (preference to those with the greatest current volume) and reports ran based off diagnosis codes assigned upon discharge from the hospital.
- Initial Selection: The top 30% of the facilities are then chosen for preliminary evaluation.
- Data Gathered: These facilities are then evaluated based off Medicare.gov data, which is a combination of State Survey Results as well as staffing and quality measure data submitted by the facility through the Caspar Report.
- Data Screening: Any facilities which had poor survey results, defined at 7 or more Quality Care and/or Mistreatment citations will be excluded.
- Facility Tours: The remaining facilities are toured by a team, which includes TriHealth Care Management, representatives assigned by the specific service line, and Senior Services. During tours an evaluation is completed by each person touring.
- Selection of Facilities: After tours are completed, the team discusses and votes on which buildings are selected based off of all the information provided by the State Surveys, information reported through CMS, and information collected through the tour.
*As geography is important to this program, a facility will be chosen based off the highest quality per region. All facilities are chosen based off the data specified in the information above.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.