Auto logout in seconds.
Continue LogoutThe current policy environment is both highly uncertain and uniquely impactful on health system finances, with a wide range of potential changes ahead that will layer on top of recent disruptions. Regulatory proposals like Medicaid work requirements and site-neutral payments could decrease revenues, while executive action on tariffs and immigration enforcement could increase costs.
Health system leaders need to assess the impact of a range of different policies — and their severity — on their organizations. We propose a four-step model to size the range of potential impacts on your organization.
Not a member? Get complimentary access to the tool.
The impact of some legislative mandates will vary state-to-state. For example, states with existing Medicaid work requirements will be less impacted than those without a provision in place. To effectively assess their susceptibility, leaders must understand their state’s context and adjust accordingly.
To capture a range of outcomes, we categorized these policies into mild, moderate, and severe scenarios based on their projected impact. Increasing severity corresponds to larger revenue reductions or expense increases:
Medicaid work requirements
No effect: No effect for states with existing requirements.
Mild scenario: N/A
Moderate scenario: N/A
Severe scenario: Severe effect for states without existing requirements.
MCO tax uniformity
No effect: Medicaid MCO tax is already equal to commercial MCO tax.
Mild scenario: State must lower Medicaid MCO tax by less than 2.5% to match commercial rate.
Moderate scenario: State must lower Medicaid MCO tax by more than 2.5% but less than 4.5% to match commercial rate.
Severe scenario: State must lower Medicaid MCO tax by 4.5% or more to match commercial rate.
Provider tax state thresholds
No effect: No effect for states without state-directed payments for Medicaid.
Mild scenario: N/A
Moderate scenario: N/A
Severe scenario: 1% reduction in total annual revenue.
Congressional and executive health policy priorities change rapidly, which means health system leaders need to track the potential impact of developing policies. Along with the policy drivers mentioned above, it is important to follow pending structural actions that could have considerable effects — as well as their range of severity. We’re keeping an eye on these pending actions because of their potential impact on changing hospital reimbursement, expenses, and overall financial stability:
- 340B: A federal program that allows eligible healthcare organizations purchase outpatient drugs at discounts.
- Tariffs: Taxes imposed on imported products.
- Medicare sequestration: Automatic decreases of Medicare payment rates to control budgetary deficits.
- OPPS claw back: Planned acceleration of CMS repayment cuts to recover almost $8 billion.1
340B
Structural change: Changes to 340B rules increase drug expenses for 340B hospitals.
Impact on health system finances:
- Drug expenses: increased costs from drug reimbursement cuts.
Mild scenario: Following an HHS survey of hospital acquisition costs, CMS reduces drug reimbursement rates by 28.5% for 340B hospitals.
Moderate scenario: Following the results of the survey, CMS reduces drug reimbursement rates by 34.7% for 340B hospitals.
Severe scenario: Following the results of the survey, CMS reduces drug reimbursement rates by 36% or more for 340B hospitals.
Tariffs
Structural change: Tariffs (and reactions to tariff uncertainty) will increase the cost of supplies.
Impact on health system finances:
- Medical supply expenses: Increased costs due to tariffs.
- Drug supply expenses: Increased costs due to tariffs.
- Construction expenses: Increased costs due to tariffs.
Mild scenario: Negotiated reductions to August 2025 tariffs or targeted exemptions to drugs and/or medical supplies.
Moderate scenario: August 2025 tariffs stand across categories.
Severe scenario: Retaliatory tariffs raise prices beyond August 2025 tariff rates.
Medicare sequestration
Structural change: Under S-PAYGO, Medicare funding will decrease, translating into reimbursement decline.
Impact on health system finances:
- Patient revenue: Reduced revenue from lower Medicare rates and curtailed patient volume.
Mild scenario: N/A
Moderate scenario: N/A
Severe scenario: Under S-PAYGO, Medicare funding will decrease by 4%.
OPPS claw back
Structural change: CMS compresses the repayment timeline for OPPS hospitals that received.
Impact on health system finances:
- Patient revenue: Reduced Medicaid reimbursement will translate into reduced patient revenue.
Mild scenario: N/A
Moderate scenario: N/A
Severe scenario: 1.5% reduction in reimbursement.
The effects of policy changes differ according to the specific characteristics of each organization For example, a health system with a higher Medicaid population will see a larger impact than another with a commercially dominated payer mix. We grouped those internal factors into two categories, which amplify or buffer the impact of different federal policies:
- Payer mix: Higher exposure to Medicare and Medicaid populations will amplify the impact of federal cuts; lower exposure will mitigate them.
- Research and grant dependence: Large research organizations and community health services for large populations will be more exposed to cuts.
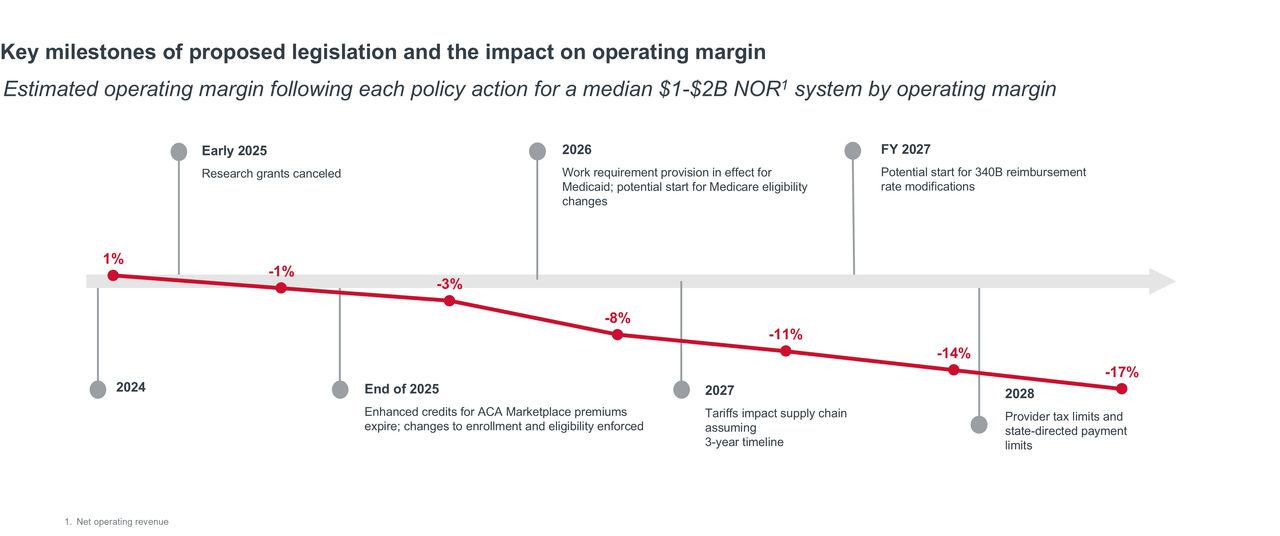
Some changes are already in effect (grant cancellations), while others will lag until future fiscal years or gradually compound in impact over time (e.g., Medicaid work requirements, eligibility verifications). As a result, leaders must also consider how the layering of policies over time will impact system finances.
| 2025 | 2026 | 2027 | 2028 | |
| Medicaid work requirements | No effect | In effect | In effect | In effect |
| Medicaid eligibility changes | No effect | In effect | In effect | In effect |
| Medicare sequestration | No effect | In effect | In effect | In effect |
| ACA cuts | No effect | In effect | In effect | In effect |
| MCO uniformity | No effect | In effect | In effect | In effect |
| Tax provider state thresholds | No effect | No effect | No effect | Severe impact |
| Tariffs | No effect | No effect | Moderate impact | Moderate impact |
| Grants | Severe impact | Severe impact | Severe impact | Severe impact |
| 340B | No effect | No effect | In effect | In effect |
| OPPS claw back | No effect | In effect | In effect | In effect |
To arrive at a range of scenarios, health system must model mild, moderate, and severe impacts on their key financial metrics (outlined in steps 1, 2, and 3), and then adjust those impacts based on their specific organizational characteristics (step 4). This scenario planning exercise should focus on the discrete policies with the greatest direct impact on financial performance drivers. By doing so, leaders can understand the different impacts of potential policy changes to plan for market- and organization-specific implications and begin to map out corrective actions.
Note: This approach focuses on the direct financial impact of health policy changes on health systems. It does not account for broader economic trends or the interaction between economic conditions and policy shifts. For example, the projected impact of Medicaid work requirements is based on historical patterns of insurance loss. It does not incorporate potential compounding effects, such as a rise in unemployment compounded by more complex Medicaid eligibility.
Prioritize action based on cumulative impact and timing
We’ve compiled a series of no-regret moves for hospitals and health systems amidst policy uncertainty. These strategies fall into five different categories:
- Strengthen planning and forecasting for resiliency.
- Evaluate purchase and purchasing processes.
- Improve revenue cycle efficiency and capture.
- Ensure workforce engagement and efficiency.
- Support providers to increase quality and access.
To dive deeper into any of these, please reach out to your client services team.
The Advisory Board data and analytics team has constructed a scenario planning model to estimate the impact of different policy drivers on hospitals and health systems of different sizes. We use data from Syntellis Market Insights to model the impact of scenarios on median operating margin. We will continue to refine our assumptions as policy changes take shape.
1 Centers for Medicare & Medicaid Services. Medicare and Medicaid Programs: Hospital Outpatient Prospective Payment and Ambulatory Surgical Center Payment Systems; Quality Reporting Programs; Overall Hospital Quality Star Ratings; and Hospital Price Transparency. Fed Regist. 2025;90(135):33476-33642.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.



