Auto logout in seconds.
Continue LogoutAs healthcare continues the transition from a system that rewards volume to one that incentivizes value, post-acute care continues to receive attention. Hospitals have responded by forming narrow networks with the highest-quality PAC providers to maximize the number of patients treated by top-quality providers. But is it enough just to identify optimal PAC providers?
Through primary research and literature review, the Post-Acute Care Collaborative has identified 10 areas that are key to an efficient post-acute episode. One of those, as outlined in the below article, reviews two case studies that highlight how deeper partnerships between acute and post-acute providers have resulted in optimized processes and streamlined care for patients.
To learn about other strategies our research indicates are key to post-acute episodes, download part two of our complete guide on the 10 Keys to an Efficient Post-Acute Episode.
Evolving industry incentives and outcomes transparency have resulted in a concerted effort among post-acute providers to strengthen clinical capabilities. However, because PAC providers care for an increasingly elderly and complex patient population, their ability to make further clinical gains is complicated.
One way hospitals can support their downstream partners is to provide training around specific patient populations and offer on-site clinician support. Collaborating to upskill post-acute staff, especially around high-risk patient populations, helps PAC providers better meet hospitals’ post-discharge expectations and placement needs.
By sharing staff with PAC providers, hospitals can give downstream caregivers an in-the-moment resource for clinical questions and help align post-acute operations with episodic goals. Further, post-acute providers’ financial incentives are usually not aligned with health system priorities related to episodic or total cost management. But extending clinical support into the post-acute setting can both improve outcomes and reinforce alignment with system goals.
Member Spotlight: Targeted Instruction and Support Improves Downstream Care for Complex Patients
Complimentary Resource
Our recommended three tier-strategy to building an optimal post-acute care networkPalmetto Health, a South Carolina-based acute care provider, found it challenging to place high-acuity Medicaid patients in skilled nursing facilities (SNF). Most local SNFs struggled to clinically manage these patients and were reluctant to accept such referrals.
However, Lutheran Homes of South Carolina, a skilled nursing and senior living provider, stepped up to the plate. Palmetto provides training for Lutheran Homes’ staff, along with a medical director and nurse practitioner to support their high‑acuity care. In turn, Lutheran Homes has developed the capability to care for these complex patients.
Lutheran Homes is now a trusted post-acute partner for Palmetto Health, and also cares for these hard-to-place patients for other hospitals in the market.
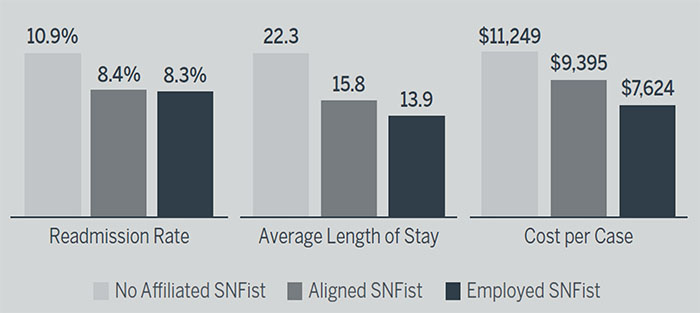
Atrius Health, an accountable care organization (ACO) based in Massachusetts, employs SNFists who practice at Atrius’s high‑volume, preferred SNF partners. Atrius also collaborates with aligned SNFists at facilities that lack the critical volumes of Atrius patients to justify an employed SNFist on site, while other SNFs in the market lack a SNFist presence entirely.
Join 100,000+ health care executives who receive our weekly emails. Subscribe now
Atrius found that, regardless of employment status, the presence of a SNFist was effective in driving quality improvement. However, a difference appeared with regard to the efficacy of employed SNFists versus affiliated SNFists in managing utilization: length of stay and cost per case is markedly lower at SNFs with employed SNFists.This illustrates a larger reality: SNFist promote improved clinical outcomes, but financial alignment is hard if there aren’t sufficient volumes to justify employing one directly.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.