Auto logout in seconds.
Continue LogoutCurrently, cancer practices utilize advanced practice providers (APPs) to support oncologists in patient management and in specialized patient support roles. This includes a variety of tasks, such as providing patient education, dictating patient notes, and handling symptom management.
But despite an anticipated increase in APPs and their growing prominence on the cancer care team, most are not used to their full potential. In 2022, only 40% of cancer practices reported using APPs at top of license. A fundamental aspect of providing top-of-license care is when APPs can perform tasks autonomously, and merely 22% of cancer programs reported using APPs predominately for independent visits.
Organizations underutilizing APPs fail to seize opportunities to maximize the time, capacity, and capabilities of all care team members to improve efficiency, patient access, care quality, and the overall patient experience.
Top of license
To practice to the full extent of one’s education and training — making the greatest contribution each individual can make — in order to maximize the value of a whole team.
For APPs, this means spending most of their time on highly skilled care activities (such as conducting independent patient visits and performing routine procedures) rather than on work that can be automated or completed by other members of the care team (such as dictating patient notes or managing prior authorizations).
APPs can and should autonomously oversee care for lower-acuity cancer patients, or those who have common or earlier stage cancers with straightforward treatment paths. Having APPs handle these tasks allows oncologists to further dedicate time to higher-acuity patients, or those with rarer or more advanced cancers with complex care journeys.
The concurrence of the following four trends makes it more important than ever to deploy APPs autonomously.
1. Rising demand and workforce challenges will deter organizational success now (and later).
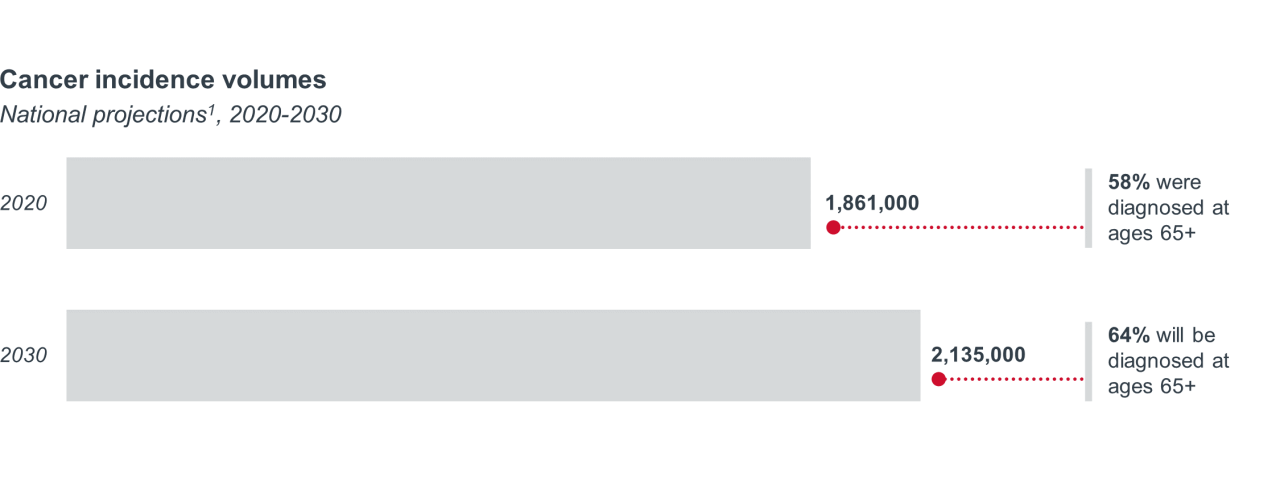
By 2030, the cancer patient population will be larger and older than it is today. Based on how care delivery teams are currently structured, there will not be enough oncologists or oncology nurses to treat these higher volumes.
Cancer workforce shortage
Projected oncologist and radiation oncologist shortage by 2025
Projected oncology nurse shortage by 20302
But this provider shortage isn’t just a future problem — it’s happening right now. In February 2023, the National Cancer Care Alliance, a network of 15 independent oncology practices across the nation, reported that every practice was desperately recruiting due to high demand. Additionally, in conversations we’ve had with cancer program leaders, nearly all of them list recruiting and retaining clinical staff as a top challenge for 2024.
2. An increasing number of cancer practices recognize APPs as high-value care team members.
More than 80% of cancer programs employ at least one APP to help ease the burdens of other care team members. This percentage is likely to get higher as the APP workforce continues to grow, with a projected increase in employment of nurse practitioners (NPs) by 45% and physician assistants (PAs) by 27% between 2022 and 2032.
3. Changing regulations will ease restrictions for APPs to practice autonomously.
Since the onset of the COVID-19 pandemic, there has been growing interest in regulatory changes that expand APP scope of practice. Today, NPs have full practice authority in 26 states, whereas PAs have broadest scope of practice in 5 states.
In the 2024 Medicare Physician Fee Schedule final rule, CMS continued to allow physicians to supervise APPs remotely through real-time audio and video until December 31, 2024.
These flexibilities allow APPs to continue practicing autonomously, especially in areas with physician shortages that would have made leveraging APPs at top of license impossible. We anticipate these flexibilities will eventually become permanent.
4. Continued sophistication of technology and AI will enable APPs to make strong clinical decisions.
One of the main fears with deploying autonomous APPs is a lack of expertise needed for independent decision-making. But future innovations in artificial intelligence (AI) and clinical decision support are likely to bridge this gap. These revolutionary tools will be advanced enough to empower APPs to make appropriate care decisions (with consultations from oncologists as needed).
Overall, cancer programs and practices must redistribute responsibilities to enable APPs to practice at top of license. Making APP autonomy nonnegotiable in your care model will improve practice productivity without requiring additional physicians.
The strategies detailed below will assist with the persistent workforce shortage, maximize oncologist time for complex patients, and reduce incidences of delayed care.
The best APP strategy for your cancer program depends on your unique business goals, staffing model, and patient demand. Here, we’ve listed five different ways to deploy APPs autonomously and the challenges they solve.
The challenge
Cancer patients experiencing symptoms often have trouble reaching their care teams due to difficulty scheduling same-day appointments with oncologists or not knowing who to turn to. As a result, these patients visit emergency departments (EDs) and are sometimes admitted inpatient (IP).
In fact, the most common entry point to cancer-related acute care is through the ED. But EDs are not always equipped to adequately support cancer patients, which drives up avoidable costs.
The strategy
Allow APPs to manage urgent care, which boosts quality for cancer patients in need of acute care compared to the general care they would receive in an ED. This also gives APPs more autonomy — an appealing incentive to APPs looking to feel more engaged in their work.
APPs managing urgent care also benefits oncologists, who can provide support to APPs as needed but simultaneously have more time to work with complex and specialized patients.
By minimizing unnecessary ED visits and IP admissions, providers can reduce total cost of care. All around, this strategy improves providers’ performance under value-based payment arrangements.
Deployment model example: Anne Arundel Medical Center
Leaders at Anne Arundel Medical Center realized that physicians were at capacity, making it difficult for them to quickly respond to nurses’ and patients’ symptom management questions. To better manage patients’ urgent needs, program leaders created a new role: one NP embedded within medical oncology whose priority is seeing patients with urgent symptoms.
To ensure appropriate use of the NP’s time, program leaders created standard care protocols, scheduling processes, and patient and caregiver education materials. In addition, they created standardized referral criteria for their phone triage nurses to use when patients call the center.
Decrease in ED visits per month on average
Decrease in inpatient admissions from ED for pain and weakness per month on average
Increase in patient satisfaction with cancer program
The challenge
Few APPs receive oncology-specific training during their education. This gap has led to physician wariness over APPs practicing at top of license, as it is unclear if APPs have the expertise required to make autonomous clinical decisions.
The strategy
Overlap APP training with oncologists to foster trust, teamwork, and cooperation, as well as a shared understanding of the medical knowledge expected of APPs to make autonomous decisions. Cancer programs can do this by offering combined educational experiences for APPs and physicians in oncology fellowship programs, allowing early-career clinicians to gain exposure to multidisciplinary care.
In addition to equipping APPs with cancer-specific expertise they may not have received in school, overlapping training also helps them understand the thought processes behind oncologists' clinical decisions.
Deployment model example: UT Southwestern (UTSW)
The UTSW Harold C. Simmons Comprehensive Cancer Center started a 12-month APP fellowship centered on postgraduate education in adult oncology. The fellowship includes didactic and clinical experiences with rotations in several oncology specialties through a multidisciplinary team approach.
Training overlaps with the hematology-oncology fellowship for their physicians to foster teamwork and cooperation between physicians and APPs. Additionally, educational opportunities like this help support workforce restructuring.
Proximity [between physicians and APPs in their fellowship] develops understanding and respect for roles and prepares both workforces for the future.
The challenge
Demand for cancer services is continuing to climb, resulting in oncologists working at capacity and managing treatment for a wide array of patients. Not all these patients have the same acuity level or require the same level of care, so some cases could be off-loaded to APPs.
On top of this, oncologists are increasingly choosing to specialize due to the vast variety of cancers and treatment innovations available, creating potential opportunities for APPs to handle more general oncology care.
The strategy
Allow APPs to independently oversee care for patients with lower-acuity and more common cancers. With APPs providing general oncology care at top of license, oncologists can simultaneously operate at top of license by providing specialized care to the most complex patients.
Secondarily, establish a strong triage system to match individual patients to the appropriate care team member for their situation. This will reduce delays in care and streamline time to appointment, helping to improve the patient experience and prevent further risk of disease progression.
Deployment model example: Allina Health Cancer Institute
At Allina Health Cancer Institute, hematology is an area with tremendous volume and capacity constraints. To improve efficiency, the hematology-oncology department implemented a system where APPs triage incoming hematology patients, pre- and post-diagnosis, with hematologist supervision. Low-acuity patients are referred to their PCP, higher-acuity patients see the APP, and the highest-acuity patients get a clinical spot with a board-certified hematologist.
Through e-consults and adequate triage, 80% of patient volumes have been redirected from needing a visiting with the hematologist.
At Allina, we have developed a triage system to ensure that care is not delayed for patients who may have more acute hematologic conditions. Simultaneously, a virtual benign hematology service addresses less urgent questions for patients who do not require a face-to-face evaluation.
The challenge
Only 3% of medical oncologists practice in rural areas. Notably, 1 in 5 rural Americans live over 60 miles from a medical oncologist, which places significant travel burden on patients and prevents timely diagnosis and treatment. The consequences of this are significant: more advanced disease at diagnosis, inappropriate treatment, worsened prognosis, and declining quality of life.
The strategy
Prioritize recruiting APPs in rural areas where physicians can remotely supervise them. Data shows that the APP supply in non-metro markets already outpaces physician supply, so APPs are well-positioned to manage care in these areas.
An increase in APPs in rural areas also minimizes the need for rural patients to travel far to receive care.
Deployment model example: Bridge Oncology
Bridge Oncology offers a radiation oncology service delivery model with specialty trained NPs who can be deployed to understaffed, rural practices. Additionally, Bridge Oncology has a proprietary platform to which member practices can subscribe, connecting providers, operational experts, and support staff to ensure quality care regardless of geographic challenges.
Bridge Oncology also offers a one-year training program for APPs, which enables them to work in any radiation oncology office. Overall, their model overcomes access gaps and removes barriers to care to provide a smoother and higher-quality care journey.
The challenge
Currently, many APPs do not have the knowledge needed to practice completely autonomously. This could change with advancements in AI and CDS tools, which could help APPs make care decisions without need for significant oncologist intervention and oversight.
The strategy
Adopt and implement AI and CDS tools to technologically enable APPs to make accurate and trusted clinical decisions for lower-acuity and common cancer cases with simpler treatment plans.
For example, we believe future AI and CDS tools will help guide APPs to a suggested course of treatment for common cancer diagnoses, taking into account clinical guidelines, patient characteristics, and other factors. New tools will also flag patients who may qualify for participation in clinical trials. This extra support and knowledge could diminish the need for oncologist supervision in APP-led cases.
Deployment model example: Massive Bio and The Oncology Institute
- Massive Bio is a company that utilizes artificial intelligence to provide concierge services to cancer patients.
- The Oncology Institute (TOI) is a provider of specialized, value-based cancer care.
Massive Bio and TOI announced a partnership in which Massive Bio will provide AI-driven precision medicine technology to “empower patients and ordering physicians at TOI with clinical decision-support” and evaluate patient eligibility for TOI’s clinical trial portfolio. The partnership aims to establish a nationwide network connecting patients to potentially life-saving treatments and trials.
Additionally, the two companies want to expand cancer research through Massive Bio’s ChatGPT-powered chatbots for oncology research. Dr. Arturo Loaiza-Bonilla, an oncologist who helped develop this technology, believes “the integration of AI-driven chatbots with clinical decision-support tools will revolutionize the way researchers access and analyze oncology data.”
Though this model does not specifically pertain to using AI to advance APP autonomy, a similar model could be used for this purpose in the future.
As your cancer program establishes or updates strategies for autonomous APP deployment, set yourself up for success by prioritizing the following three actions:
1. Have a clear strategic goal for elevating APPs to top of license.
Even in the most optimally scoped role, APPs won't be able to adequately support the cancer program unless you also lay the groundwork to set them up for success.
Before rapidly hiring APPs, first determine what challenges you’re trying to solve. Then prioritize the challenges to rightsize how many APPs you need, where you need them to focus, and what program goals you most need them to support.
2. Prepare your organization for APPs to practice autonomously.
After assessing preexisting workflows, staffing, and cultural challenges at your organization, the next step is intentional investment in educational and engagement opportunities about the value of APPs. This promotes care team collaboration and eases worries about APP care management, expertise, and credentials. Below are some questions to consider when educating patients and your workforce about APPs:
- How will you prepare the rest of your care team for shifting role responsibilities?
- How will you demonstrate that elevating APP role responsibility benefits physicians and patients alike?
3. Align physician and APP deployment, training, compensation, and leadership.
This will enable you to maximize the return on your investment in APPs. For more, read our research on deploying APPs autonomously.
1Volume projections come from Mariotto AB, et al., while proportions of patients diagnosed at age 65 and older come from Advisory Board’s Cancer Incidence Estimator.
2Based on proportion of nurses certified in oncology in 2017.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.



