Auto logout in seconds.
Continue LogoutOverview
Nurse leaders are under pressure to deliver care team value—which means they're torn between cutting costs and providing high-quality nursing care. But to build a high-value care team, they must focus on both.
This study identifies three inefficiencies that plague care teams and includes strategies to achieve the right balance between dollars spent on staffing and quality.
Traditional strategies no longer enough
Most traditional efforts to drive care team value have focused on just one side of the value equation—either inputs (for example, hours per patient day or salaries) or outputs (for example, high-quality patient care or strong performance on nurse-sensitive indicators).
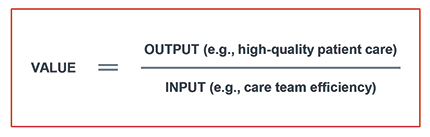
It's time to change the conversation. Nurse leaders looking to build a high-value care team must take a balanced approach, providing the highest possible quality care for every dollar spent on staffing. And the time is right: with nearly one million nurses reaching retirement age in the next 10-15 years, nurse leaders have a unique chance to carry out these changes.
Read more about the value equation
Three near-universal opportunities for increasing care team value
But where are your biggest opportunities to drive value? There are three inefficiencies that plague nearly all care teams.
- First, there is overreliance on bedside RNs to complete work that support staff or other non-RN care team members can safely accomplish. Nurse leaders should ensure all care team members are working at the top of their license—and then consider changing the proportion of bedside RNs or trading a bedside nursing position for an expert RN role.
- Second, uncoordinated interprofessional care often leads to duplicative efforts and wasted resources. The most effective organizations closely align all care teams' goals and workstreams, encouraging real-time collaboration whenever possible.
- Finally, many organizations deploy a "one-size-fits-none" care team, an approach that usually fails to meet high-risk patient needs and may over-serve low-risk patients. We've outlined a five-step process to help hospital leaders scale care team staffing to patient need.
Explore the three root causes of inefficient care teams
Three paths to value—and the moves to get there
To help you fight these inefficiencies, we've identified three critical paths to greater care team value—and provided detailed guidance to help you implement them at your organization.
Align Interprofessional Goals and Work
Deploy the Minimum Core Team and Selectively Scale Up Support
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
