Auto logout in seconds.
Continue LogoutPassed in 2015, MACRA is arguably the most monumental legislation for Medicare physician payment from the last decade.
MACRA combines parts of the Physician Quality Reporting System (PQRS), the Value-Based Payment Modifier Program (VBM), and the Medicare Electronic Health Record (EHR) Incentive Program into a single, points-based system—the Merit-Based Incentive Payment System (MIPS).
Not surprisingly, there’s a lot of confusion surrounding how MIPS impacts health care providers. As a field sales rep, an account executive, a medical liaison, or a customer service manager in the health care industry, you need to know the ins and outs of MACRA, including how CMS holds physicians accountable for the quality of care they deliver.
In the last part of our five-part educational series, you’ll learn important program acronyms and definitions, a breakdown of two new payment tracks—MIPS and the Advanced APM—and how MACRA continues to evolve. Check out the below article to get a preview and download part five of our complimentary resource to learn more.
Infographic: 5 Things Everyone Should Know About MACRA
What is MACRA?
While there are a lot of parts to MACRA, two important changes include:
- It holds physician Medicare base payment at near zero growth over the next 10 years, which effectively nullified a series of historic fixes and adjustments to physician reimbursements (such as SGR). This sets the stage for a new physician reimbursement model.
- It authorizes the Department of Health and Human Services (HHS) to implement value-based strategies aimed at improving costs and quality of care to CHIP and Medicare beneficiaries.
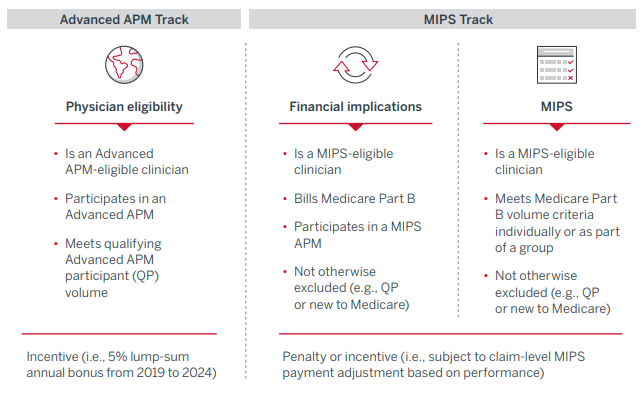
The result is the creation of two new payment tracks for all physicians who bill through Medicare Part B. These two tracks, called the Merit-Based Incentive Payment System (MIPS) and the Advanced Alternative Payment Model (Advanced APM), determine the rate of increase for physician base payment. More importantly, they determine whether a provider is eligible for certain bonuses or penalties.
Overview of Advanced APM and MIPS tracks under MACRA
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.