Auto logout in seconds.
Continue LogoutA new study reveals that, of more than 400,000 nurses who quit their jobs in 2018, nearly one-third cited burnout as their reason for leaving, according to a study published this month in JAMA Open Network.
Our take: Building a flexible nursing workforce
Study details
For the study, researchers at Emory University conducted a secondary analysis of survey data to measure rates of nurse burnout in the United States and identify risk factors associated with nurse burnout. The researchers analyzed cross-sectional survey data collected by HHS' Health Resources and Services Administration from April 30, 2018, to Oct. 12, 2018, for the agency's National Sample Survey of Registered Nurses.
The data included 3,957,661 respondents, with a mean age of 48.7 years old. Majorities of the respondents worked in hospitals (63.7%), were women (90.4%), were white (80.7%), and were full-time nurses (82%). Most of the respondents lived in the South (40.3%) or Midwest (24.8%).
Why 418,769 nurses left their jobs
According to the study, 10.6%—or 418,769—of the respondents reported that, as of the date they responded to the survey in 2018, they had left the job they had held on December 31, 2017.
Of those nurses, 31.5% reported burnout as a reason for leaving their position, making it the third most commonly cited factor. Other top reasons for leaving included a stressful work environment, lack of good management or leadership, inadequate staffing, and finding better pay/benefits elsewhere.
The share of nurses who cited burnout as a reason for leaving their jobs varied widely between states, from a low of about 17% to a high of about 48%. (The study reported state-by-state results only in ranges, rather than citing a specific burnout percentage for each state.)
"The lower reported rates of nurse burnout in California and Massachusetts could be attributed to legislation in these states regulating nurse staffing ratios," the researchers explained. "The high rates of reported burnout in the Southeast and the overlap of burnout and inadequate staffing in our findings could be driven by shortages of nurses in the states in this area, particularly South Carolina and Georgia."
The researchers also found that, out of the broader pool of nearly 4 million nurses surveyed, nearly 17%—or 676,122—reported having considered leaving their position. Among those, 43.4% identified burnout as a reason they would leave their job.
The share of nurses who reported considering leaving their jobs due to burnout varied between states, with relatively low percentages doing so in California, Washington, and New York and relatively high percentages doing so in Utah and New Mexico.
What does this data mean for nurses today?
Although the researchers examined data collected before America's coronavirus epidemic took hold, they acknowledged the "ever-growing stress associated with the … [epidemic] … could leave the [United States] with an unstable nurse workforce for years to come."
The researchers argued, however, that there are ways to address the factors associated with burnout.
"Legislation that supports adequate staffing ratios is a key part of a multitiered solution," the researchers wrote. "Solutions must come through system-level efforts in which we reimagine and innovate workflow, human resources, and workplace wellness to reduce or eliminate burnout among frontline nurses and work toward healthier clinicians, better health, better care, and lower costs" (Kunzmann, HCPLive, 2/4).
Nurse burnout didn't start with Covid-19. (And it won't end with Covid-19, either.)
 By Katherine Virkstis, Managing Director and Senior Research Partner
By Katherine Virkstis, Managing Director and Senior Research Partner
Nurses have been struggling to bear the weight of the Covid-19 crisis for nearly a year now. But as this newly released data reveals, nurse burnout was already a challenge long before the pandemic began.
In some ways, that's puzzling. Nearly every clinical leader I know is deeply focused on engagement and wellness of their teams. So why are so many nurses still burned out—and even leaving the profession?
In my team's pre-Covid research, we found a potential solution by going back to Maslow's Hierarchy of Needs. The hierarchy proposes that basic needs lie at the bottom of Maslow's pyramid. I think of these needs in the way humans need air, food, and water to live. These basic needs must be met before a person can fulfill their higher-level needs, such as self-actualization.
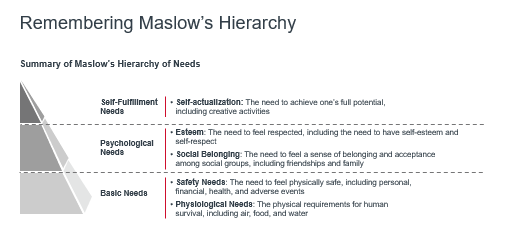
Our research revealed, even before the pandemic, most nurse leaders were focusing their efforts on the top of the pyramid, aiming to help nurses work creatively and achieve their full potential. It's an important goal, but if you overlook fundamental needs, you could be unintentionally missing what's driving nurses into burnout.
So from a clinician's perspective, what are those basic needs at the bottom of the pyramid? Our pre-pandemic research identified four key "cracks" in the foundation:
- Safety threats in the workplace;
- Compromises in care delivery;
- A lack of time to recover from traumatic experiences; and
- Feeling isolated, even when surrounded by people all day.
These are the exact same challenges the clinical workforce is facing today amid Covid-19—just turned up by a factor of a thousand.
So instead of focusing on higher-level aims like "engagement" right now, you should instead aim to address the foundational problems undermining your team's resilience. In our emotional support resource library, you'll find actionable resources to help you:
- Ensure nurses are safe and feel safe at work;
- Be transparent about how you are staffing the mission;
- Make emotional support opt-out, not opt-in; and
- Carve out time for personal connection.
And don't forget to focus on your own resilience. You need to put on your own "oxygen mask" first—to take care of yourself before you can support others. The current environment is volatile, uncertain, complex, and ambiguous. Allow yourself to be a vulnerable leader, and show staff that it's okay to not have all the answers, to need help, or not be at 100% every day.
The Covid-19 crisis will end someday, but the challenge of clinician burnout will remain. You'll need to prioritize your team's resilience for years to come.
Hear more from Katherine Virkstis on the recent episode of Radio Advisory, "Resilience: Not just a pandemic buzzword—and not the same as engagement"
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
