Auto logout in seconds.
Continue LogoutCreating simple communication strategies, working with allies, and easing how members interact with their plans are three strategies our research indicates are critical to improving member engagement. Our fourth key to building stronger relationships with your members is to create processes that act on a member’s behalf.
There are a variety of ways to assist your members, while simultaneously creating and building a trusting relationship. Below we outline two case studies in which health plans took the initiative and took care of their members. First, we outline how Passport Health makes sure their members have a Primary Care Physician (PCP), and then we outline how Caremore helps their members get to medical appointments. In both instances, the health plan stepped up, supported their members, and made sure their members’ health was a priority.
To read similar case studies and learn other strategies that our research indicates is critical to member engagement, download our complimentary resource Shattering the Member Engagement Myth Part Two: Health Plan Diplomacy.
With their vast resources, communication systems, and data warehouses, plans can have a huge impact on consumer behavior. While plans must use their power selectively—too much force can alienate members or sour relationships—plans are also in the unique position to assist members in making sound health-related decisions and to support them in accessing care.
Case study: Passport Health Schedules for Members
Passport Health, a 177,000 member Medicaid plan in Kentucky, is using a specialized team in their call center to proactively connect members with primary care physicians.
When members are on the phone with Passport, the call center representative makes sure the member has a PCP, and if they don't, schedules an appointment immediately.
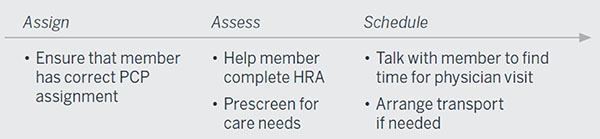
So far, 800 new members have gotten a PCP appointment through Passport scheduling and other incentive programs.
Case study: CareMore gives members a ‘Lyft’ to their PCPs
CareMore is an integrated health plan and delivery system that provides care for enrollees in Medicare Advantage and Medicaid health plans in California, Nevada, Arizona, Virginia, Tennessee, Iowa, and Georgia. When CareMore found that its members often faced significant wait times with its existing transit services, it looked at options outside of traditional health care transportation—and built a partnership with the ridesharing service, Lyft, to make non-emergency medical transportation (NEMT) faster for members and more affordable for the plan.
CareMore and Lyft built the new service with the member perspective in mind at every step—starting when members request a ride.
Since many of their members are unfamiliar with smart phones (or don't have them), CareMore set up a dedicated transport call team to intake member requests. The representatives collect information about the location, destination, timing, and any special needs.
CareMore then transmits the information to its transportation benefit manager, National MedTrans Network, which works with Lyft to schedule the ride:
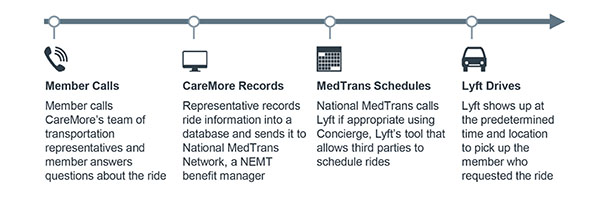
The program was initially run as a pilot among Medicare Advantage and dual-eligible members in California. The pilot resulted in shorter wait times, lower costs, and higher satisfaction when compared to traditional NEMT, according to data published in JAMA. The data was based on 497 NEMT rides between May 2016 and June 2016.

Because of these promising results and continued good performance, CareMore is expanding its program to more of its populations.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.