Auto logout in seconds.
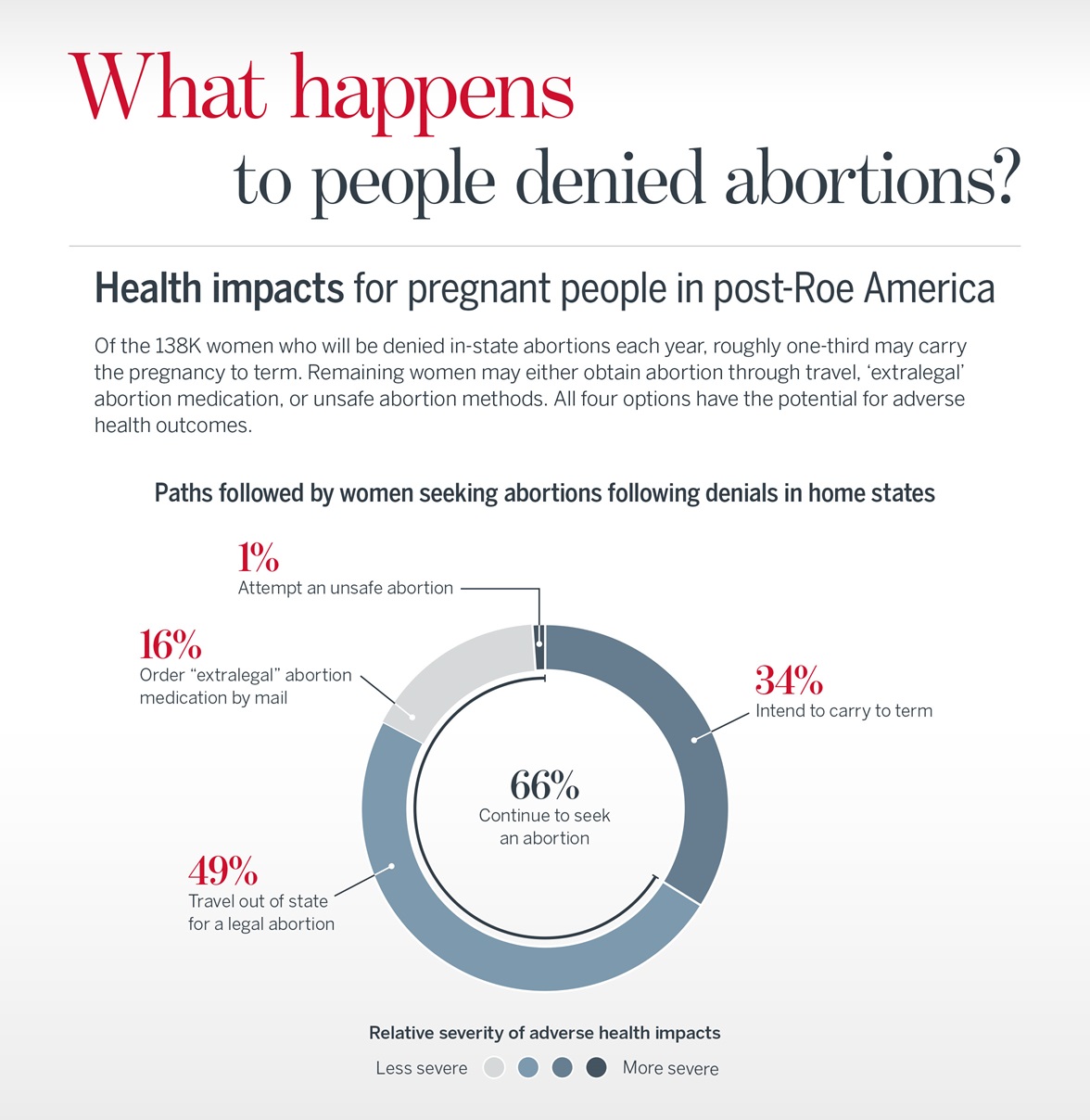
Continue LogoutAn estimated 138K women per year will be denied abortions in their home states following the overturning of Roe v. Wade. This population will have four options, and each carries the risk of adverse health outcomes and behaviors. To effectively adapt their maternal and reproductive health service offerings, stakeholders must understand the forecasted outcomes and volumes for each pathway below:
- Carry the pregnancy to term
- Travel out of state for legal abortion
- Order “extralegal” medication abortion by mail
- Attempt an unsafe abortion
For an overview of evidence-based health outcomes associated with unwanted pregnancies, download our comparison chart found in the right rail of this page.
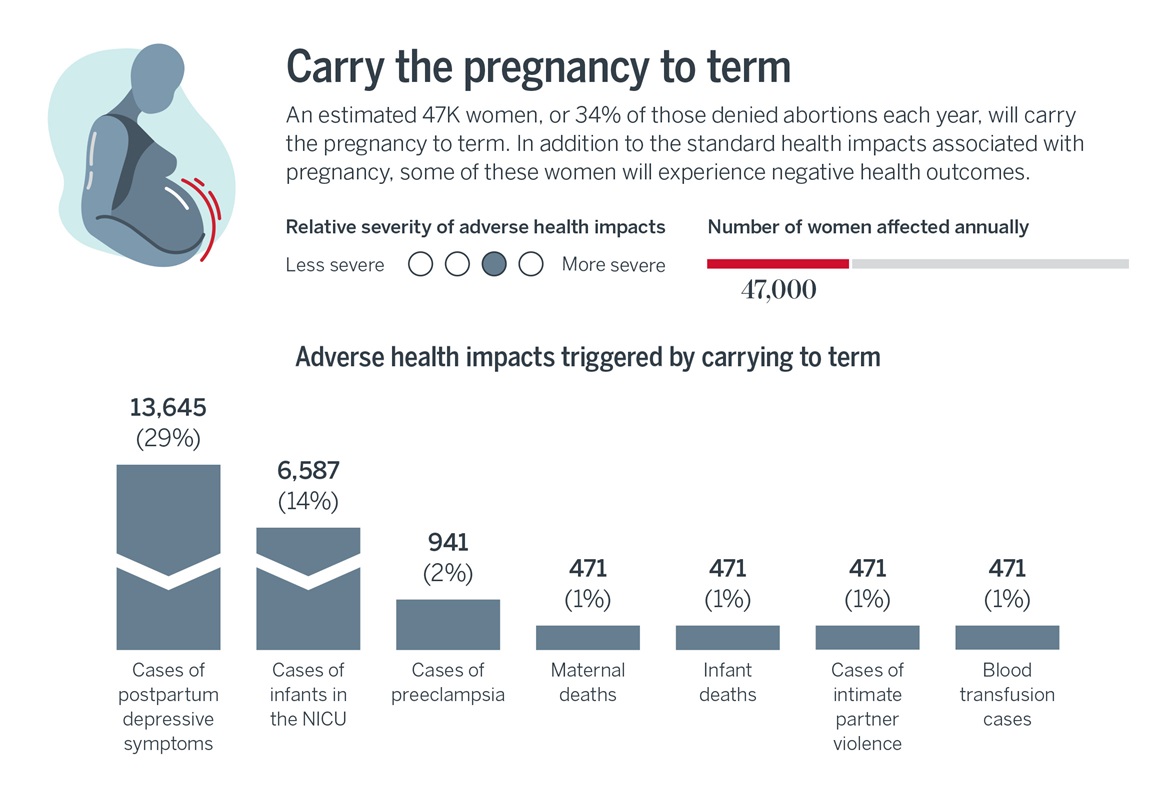
Other potential outcomes include rare but potentially life-threatening maternal health complications, including eclampsia and postpartum hemorrhage, and common but underreported mental health conditions like low life satisfaction/self-esteem and postpartum depression.
Those with unwanted pregnancies are also more likely to experience intimate partner violence (IPV) and less likely to engage in recommended perinatal practices, such as taking folic acid, attending prenatal care visits, and breastfeeding. Not engaging in these practices increases the risk of birth deformities, pregnancy complications, and breast and ovarian cancer. This contributes to worsened newborn health outcomes among pregnancies that result in childbirth.
Just as the pandemic energized commitments to advance health equity, the overturning of Roe v. Wade should serve as an industry-wide wake-up call to prevent and better manage high-risk pregnancies. The CDC recommends health plans reimburse providers for the full range of contraceptive methods to prevent the health risks of unintended pregnancies. Providers and payers also have an opportunity to proactively identify high-risk pregnancies, enhance the quality of perinatal care, and ultimately improve birth outcomes for those carrying unwanted pregnancies to term.
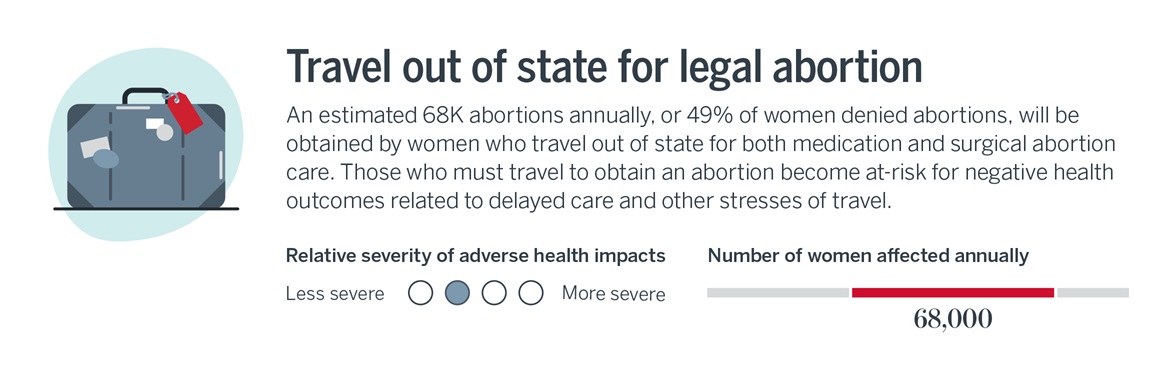
Women who must travel for abortions are more likely to delay care and receive abortions at later gestations, which increases various health risks. For example, women who travel farther for abortions are 2.3 times as likely to need an emergency department visit compared to those with care available locally.
Traveling for an abortion necessitates managing unforeseen costs, privacy concerns, logistics, and potentially childcare needs – additional stressors that may contribute to the negative mental health impacts imposed by state abortion restrictions.
To help offset the burdens associated with traveling for an abortion, payers and major employers have already committed to offering travel reimbursement for employees and their families. Additionally, Cigna is expanding its offerings to include not only abortion care, but also gender-affirming and behavioral health services in states with restricted access. We’ll be tracking how other purchasers respond in these areas, especially as data becomes available regarding the different needs and risks of those who must travel for medication versus procedural abortion.
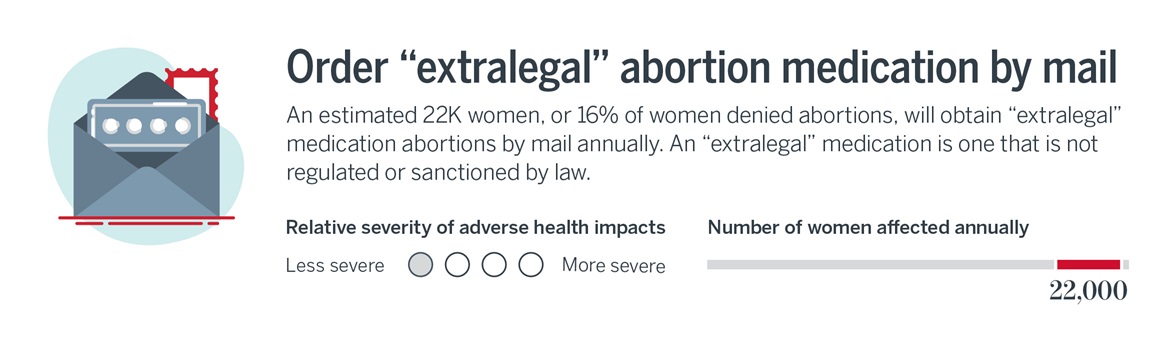
“Extralegal” medications are often ordered through international telehealth companies like Aid Access, whose doctors face little legal risk from state laws in the U.S. While individuals may struggle to verify the efficacy and safety of these internet companies, the limited, available literature suggests only a small portion of women will experience health complications. One study found that 1% of Aid Access patients experienced serious adverse events, requiring blood transfusions and IV antibiotics.
Based on the growth of medication abortions – the CDC found that from 2004 to 2019, medication abortions at nine weeks gestation or less increased by 219.6% – and the increased popularity of international telehealth companies, providers should watch how the use of “extralegal medications” may increase to gauge and respond to any emerging health care needs.

Unsafe abortion attempts conducted with risky and invasive methods could result in hemorrhage, infection, uterine perforation, and other damage to the genital tract and internal organs. Other health consequences include anemia, pain, prolonged weakness, and mental health distress. In severe cases, those attempting unsafe abortions may require a hysterectomy or develop chronic complications such as pelvic inflammatory disease, inflammation of the reproductive tract, and secondary infertility. These unsafe abortion attempts could also increase abortion-related emergency department visits and maternal mortality.
The anticipated increase in patients attempting unsafe abortions may be slight, but cross-industry stakeholders should track the impact on patient health and care utilization to scale their responses appropriately. As restrictions and their impacts will be localized, some hospitals, emergency departments, and urgent care centers may need to revisit protocols, triage and navigation resources, and staff training in the coming months and years.
Now more than ever, invest attention and resources in maternal health outcomes
Given limited data sources, our forecasts likely underestimate the magnitude of adverse health outcomes associated with abortion denials following the overturning of Roe v. Wade. Regardless, they echo long-standing calls for cross-industry leaders to advance maternal health equity and better meet the needs of pregnant people, including those who must choose an alternative to in-state abortion.
Note: Although a small proportion of abortions and pregnancies occur among transgender men or nonbinary people, we are limited to using abortion and population counts of women of reproductive age produced by the CDC and U.S. Census Bureau.
Contributors: Phoebe Donovan and Emily Heuser.
In addition to the business implications for all health care stakeholders, we are researching how to support the clinical workforce, and the impact on pregnant patients and their families.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.

