Auto logout in seconds.
Continue LogoutThe challenge
Health systems can achieve growth, quality, and cost benefits from service consolidation. But internal politics often hold back decision-making and prevent rationalization. To overcome that challenge, system leaders typically focus on gaining buy-in for rationalization from skeptical stakeholders, rather than engaging others in the decision process.
The organization
Sinai Chicago is composed of two acute care hospitals, a post-acute freestanding rehab hospital, and multispecialty medical group. The north campus acute care hospital is an academic teaching facility with a high-level trauma center. The south campus acute care hospital was traditionally viewed as a bread-and-butter community site but was facing volume leakage and financial unsustainability.
The approach
In late 2019, Sinai engaged system and community stakeholders in a participatory and transparent change process rooted in the system’s larger transformation initiative. This culminated in consolidating services from south to north campus to best enable Sinai to achieve its vision for the future as soon as possible.
The result
As of 2021, Sinai has achieved more than $45M in cumulative margin improvements with $12.5M savings from rationalization services between north and south campus. Furthermore, incorporating a wide base of stakeholders has eased the decision-making process for future rationalization decisions.
How Sinai Chicago’s participatory process enabled rationalization
Sinai built a decision-making and implementation structure that engaged stakeholders across and outside of the system to address underlying issues identified in the system’s transformation vision. Stakeholders and system leaders worked together to identify viable steps to support Sinai’s transformation goals, eventually settling on service rationalization.
The four steps
By following four steps, Sinai consolidated services while ensuring that relevant stakeholders understood why rationalization was taking place and could prepare for the changes in advance.
Historical performance and new goals necessitated change
In 2018, Sinai Chicago faced a host of challenges, including dilution of commercial coverage, shifting demographics and payer mix, and a renewed focus on population health. More specifically, Sinai’s south campus had poor financial performance and was losing patient volumes to competitors. The system’s financial, quality, safety, and service priorities could be achieved only with significant reorganization. In response, Sinai Chicago’s leadership team launched a transformation campaign focused on three goals:
- Become the provider of choice marked by top decile quality and service
- Drive greater than $75M in margin improvements
- Achieve “systemness”
Need and urgency from transformation process opened door to service rationalization
In launching the transformation initiative, Sinai Chicago’s leaders created awareness of challenges the system faced, as well as the goals they wanted to achieve. By anchoring its change efforts in the goal of better serving its community, Sinai established a clear vision for its staff. Individuals understood that Sinai aspired to be the health system that not only provided the best patient experience but also was financially sustainable and able to operate cohesively. The transformation initiative both established the status quo as untenable and focused stakeholders on achieving a new vision for the system.
Sinai also wanted to meet their objectives within five years, which meant that they needed to act quickly. Stakeholders became open to substantial changes that would improve quality and decrease inefficiencies, such as service rationalization.
Participatory process focused on solving problems and proposing solutions
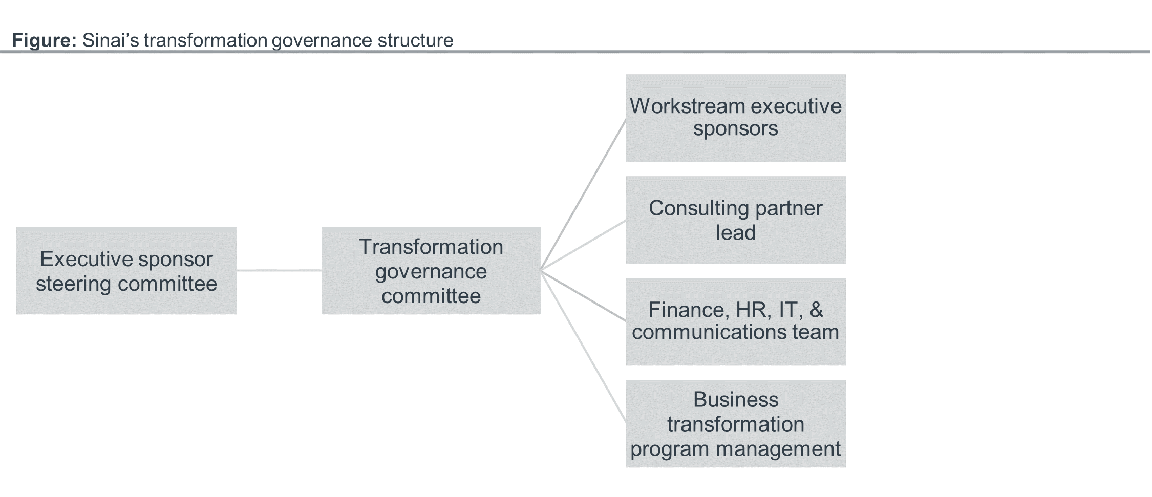
With consensus on the problems and a clear vision for the future, Sinai’s system leaders established a participatory change process. System leaders served alongside service line leaders, physicians, and other stakeholders across the organization in a transformation governance structure.
These groups compared options and evaluated the consequences of different changes. A steering committee of executive sponsors supervised transformation governance teams overlooking specific workstreams. Service line, administrative, and physician leaders participated in committees of their choice. The governance committee or workstream leads also invited additional members as needed.
System leaders did not presuppose rationalization
The working groups determined the right next steps for the system. Notably, system leaders did not assume that rationalization was necessary for transformation. In fact, working groups identified a host of additional actions that Sinai Chicago has since implemented, including standardizing call structure in Sinai’s emergency department and heart and vascular services, as well as integrating the diverse physician groups into a larger Sinai medical group.
The working groups also identified options to address underperformance at south campus and the need for Sinai to integrate into a single system. Ultimately, they recommended consolidating obstetrics and women’s health, surgical services, gastroenterology, oncology, and heart and vascular services.
Because they played a critical role in identifying the solution, service line, and physician leaders became proponents for rationalization. In a top-down process, those same stakeholders could have been defensive about any changes occurring. System leaders would then have to persuade skeptics and overcome resistance. While Sinai’s approach did not achieve universal buy-in on the service rationalization decision, everyone involved in the process could understand what was taking place and share their opinions.
Change champions emerged out of individuals formerly against rationalization changes
Sinai Chicago’s system leaders dedicated personal time to stakeholders most skeptical of rationalization. System leaders held continuous conversations centered around Sinai’s need for transformation, backed by performance and financial data, and how to achieve it.
For example, one of Sinai’s private physician group partners initially opposed any rationalization effort that affected their services. Through a series of one-on-one conversations with transformation leaders, the group eventually became supporters of the initiative. They recognized both the need for change and the opportunities it created for them. Instead of skeptics, the group then acted as change champions who could articulate to their peers what the system wanted to achieve and how to work with system leaders through the process.
Sinai’s transparency and open communication, at an institution-wide and grassroots level, included many individuals in the decision-making process and confronted resistance.
Early, open communication included those that could not actively participate in decision-making
While the transformation initiative was highly inclusive, not everyone could be involved. Sinai Chicago’s system leaders actively publicized how they were making decisions rooted in the transformation effort, including on rationalization. The system’s communication team created a messaging plan for those outside the process to build awareness of why the system needed a change, how they were structuring their decision process, and how it progressed.
The system relied on a variety of channels to get out the message, including around-the-clock town halls, emails, and updated documents covering frequently asked questions. By communicating early and often, the team was able to spot pushback and connect stakeholders with system leaders for additional support. Furthermore, Sinai’s openness in communications ensured that no stakeholder would be caught off guard by the changes happening.
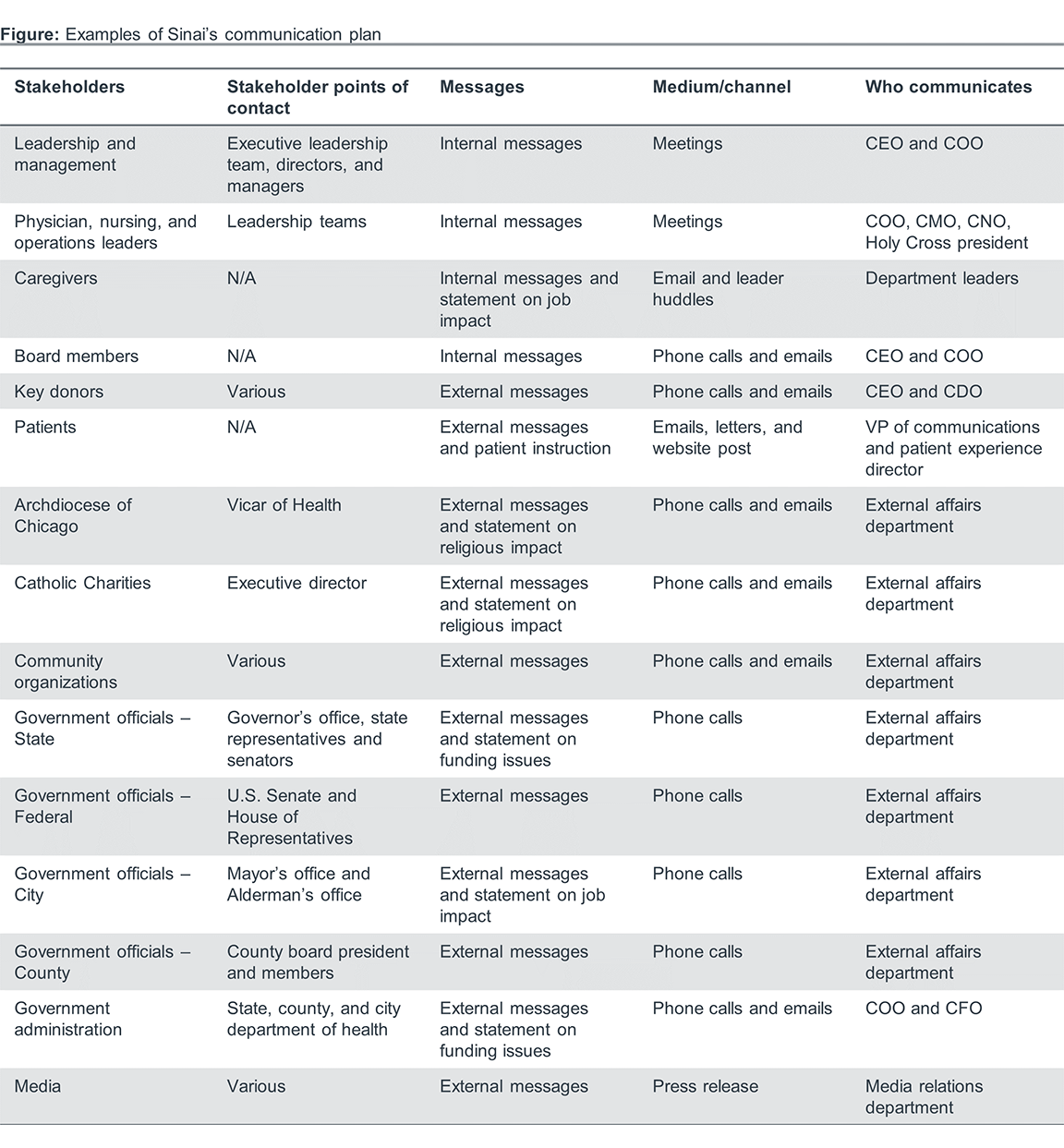
Individualized messaging addressed stakeholder’s unique concerns
In addition to providing generalized messaging, the communication team outlined a tactical approach for each segment of Sinai Chicago’s internal and external stakeholder categories. This included over 70 different stakeholders.
For each stakeholder segment, the communication team developed a plan that covered the reasons for change, how Sinai made the decision, how it would affect the constituent, and how the constituent could get involved.
Transparent communication with community stakeholders
Those communication plans included external stakeholders. Sinai Chicago wanted to build buy-in from the community for service distribution changes. For instance, Sinai’s leadership team met with several different local and federal government officials to ensure that they were fully aware of the changes, which prevented a negative political reaction. Sinai also worked with the local archdiocese because of its strong partnership with the south campus known as Holy Cross Hospital, a long-time Catholic health care institution.
By giving political leaders, representatives of the archdiocese, and other community leaders a chance to voice their concerns and stay informed of the process, Sinai ensured those leaders would be able to explain the changes to their communities.
Stakeholder participation helped empower internal and community stakeholders
Sinai’s leadership team knew that they could not independently anticipate all the operational implications of service distribution. To prepare for the resulting changes from rationalization, Sinai’s leaders asked stakeholders affected by the transformation process for their input. As a result, those stakeholders were able to provide diverse and on-the-ground perspectives on the actions needed to make rationalization a success.
Sinai’s leadership team contacted different stakeholders and community groups to help plan the operational changes resulting from rationalization. Specifically, Sinai hosted patient advisory councils with assistance from Sinai Community Institute, the system’s social services arm, which focuses on community outreach and engagement. Given that Sinai is one of the largest safety-net systems in Chicago, these meetings helped identify ways to reduce the impact on patients close to south campus and retain them throughout and after service changes. For instance, the patient advisory council realized that many patients near south campus lacked transportation to north campus. To address that gap, Sinai Chicago built a bus system connecting patients to north campus, ensuring that patients would not lose access to care.
Additionally, Sinai spoke with other affiliated health care facilities to avoid disruptions to referrals from community providers. The feedback Sinai received strengthened the original rationalization plan to fit the needs of the community.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.


