Auto logout in seconds.
Continue LogoutWhen it comes to care management, early identification of a high-risk member could result in both a more healthy member and significant cost savings. While there are a great number of high-risk populations that health plans track, one particularly important population is expectant Mothers. Below, we delve into how Health Plan Partners (HPP) used data to identify their population of high-risk pregnancies and the care management program they created to provide proactive support.
Often, the hardest part of care management is actually identifying the members who need it. A notable high-risk population is expectant mothers, and rightfully so. According to Fair Health, the average price for having a baby in the US can range drastically from $5,000 to $28,500. Further, due to the increased rates of C-sections in the US, the overall costs associated with births are expected to increase.
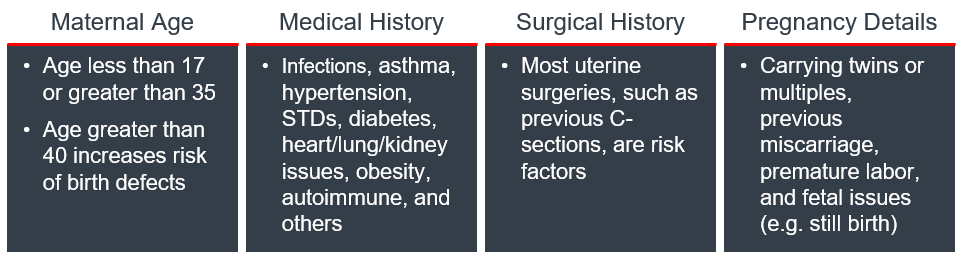
There are four types of risk factors that could bring a relatively low-cost pregnancy to a high-cost, high-risk pregnancy: maternal age, medical history, surgical history, and pregnancy-related issues.
Table 1: Factors that can contribute to a high-risk pregnancy
But even with the risk factors outlined in the literature, it is challenging for plans to identify high-risk pregnancies for three main reasons:
- Plans are unable to predict pregnancies from past claims as they can for most illnesses
- Pregnant member data is not in a centralized source, but rather spread across multiple sources
- Plans only have 9 months to both identify the member and intervene
Health Partners Plan, a Medicaid plan based in Pennsylvania, recognized these issues and sought to not only identify their high-risk, expectant mothers, but to also create a care management program to support them: The Baby Partners Program.
First, HPP’s data analytics team identified the available data sources that could help them both identify newly expecting mothers and potential risk-factors. Next, they created an automated weekly data pull that would consolidate all relevant data sources to create a list of high-risk pregnant members. This list is sent to the Baby Partners care management team. Within 24 hours of receiving the list, the Baby Partners Team proactively reached out to these members to offer tailored information and resources to help ensure the health of both the mother and the baby.
Within the first year of the program’s inception, over 1000 expectant mothers were contacted and HPP saw a 14% reduction in risk of low birthweight babies, 20% increase in post-partum office visits, and $1.5M in savings in the first 3 months for participating babies.

The results speak for themselves. In fact, the numbers are so impressive that other plans have leveraged this strategy. This is just one statistic that resulted in immediate expansion of this prenatal care management program.
About the Health Plan Advisory Council
The real-world tactics and strategic guidance health plans need to solve their current challenges and make smart investments for the future.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.

