Auto logout in seconds.
Continue Logout2020 saw the biggest spike in virtual visit utilization, accelerating the telehealth implementation timeline of many organizations by 2-5 years. With a hopeful rollout of the vaccine on the horizon, health plan leaders must turn their focus to integrating virtual care in a sustainable, data-driven way that centers around what their members want. Advisory Board surveyed over 3500 consumers in April right after the pandemic hit the US to determine their telehealth preferences. We’ve highlighted three key takeaways for all health plan leaders to consider as they plan their virtual strategy for 2021 and beyond.
1. Top virtual visit utilizers: individual market members, high-cost members, and members with prescriptions.
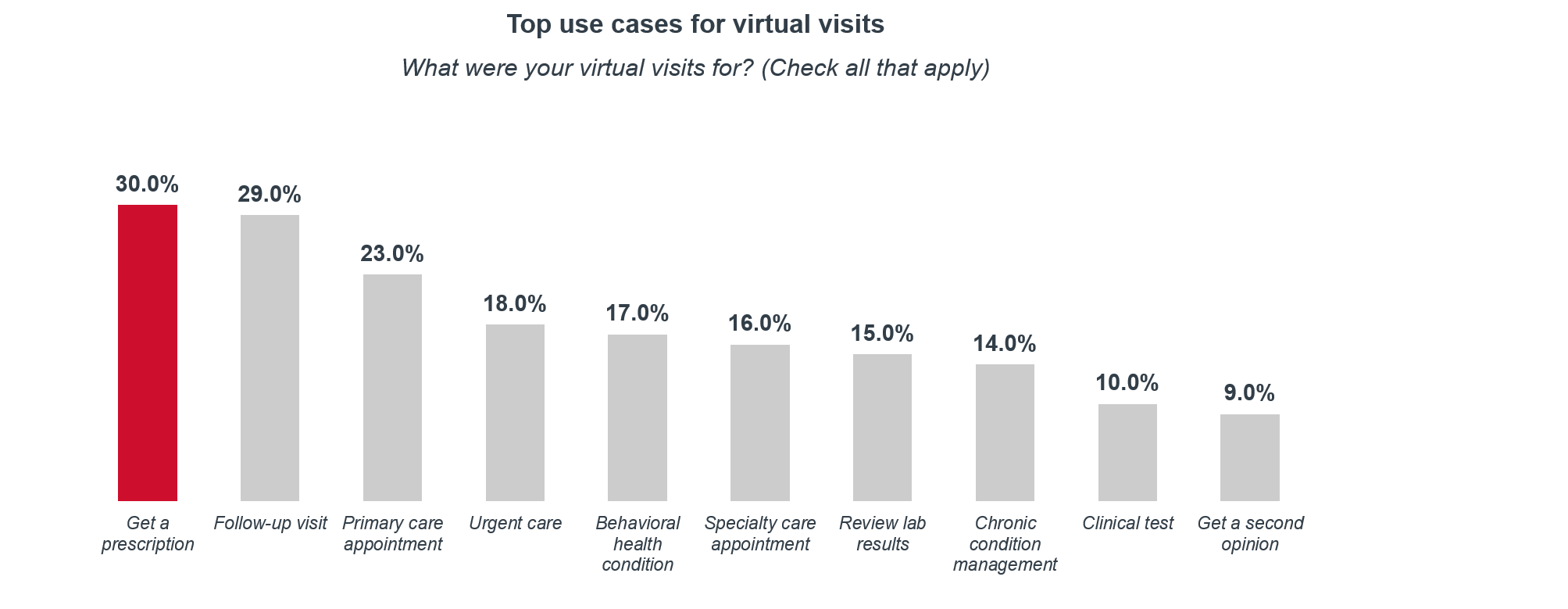
It’s no secret that Covid, and the resulting shutdowns, stay-at-home orders and a risk-averse shift in consumer habits has resulted in the increased acceptance for alternative modes of care such as virtual visits (VV). Utilization has been especially high in the individual market with 46% of members saying they have used a VV before. In addition, it is not just the young and healthy using virtual visits. 40% of high-cost members have used VVs before, compared to 29% of the general population. Lastly, of the members who have had a virtual visit, the top reason was to get a prescription followed closely by follow-up visits.
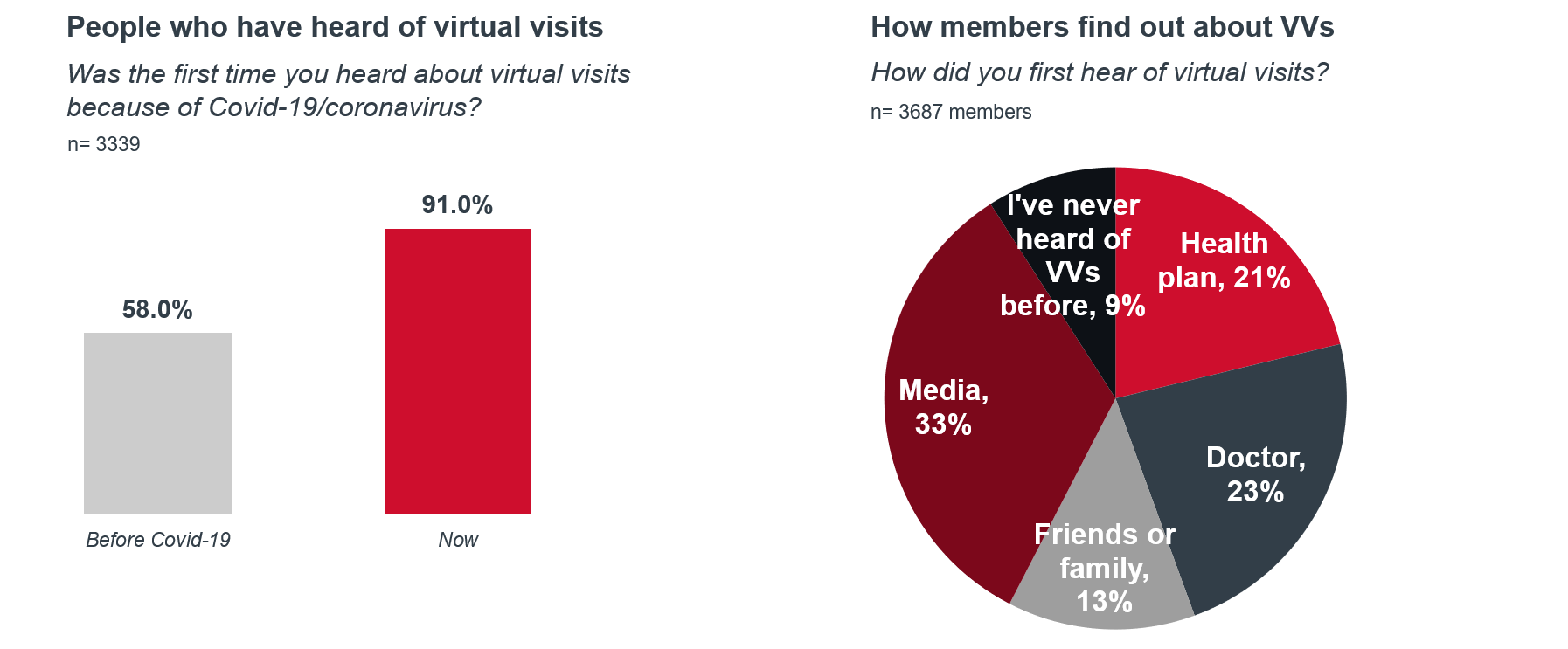
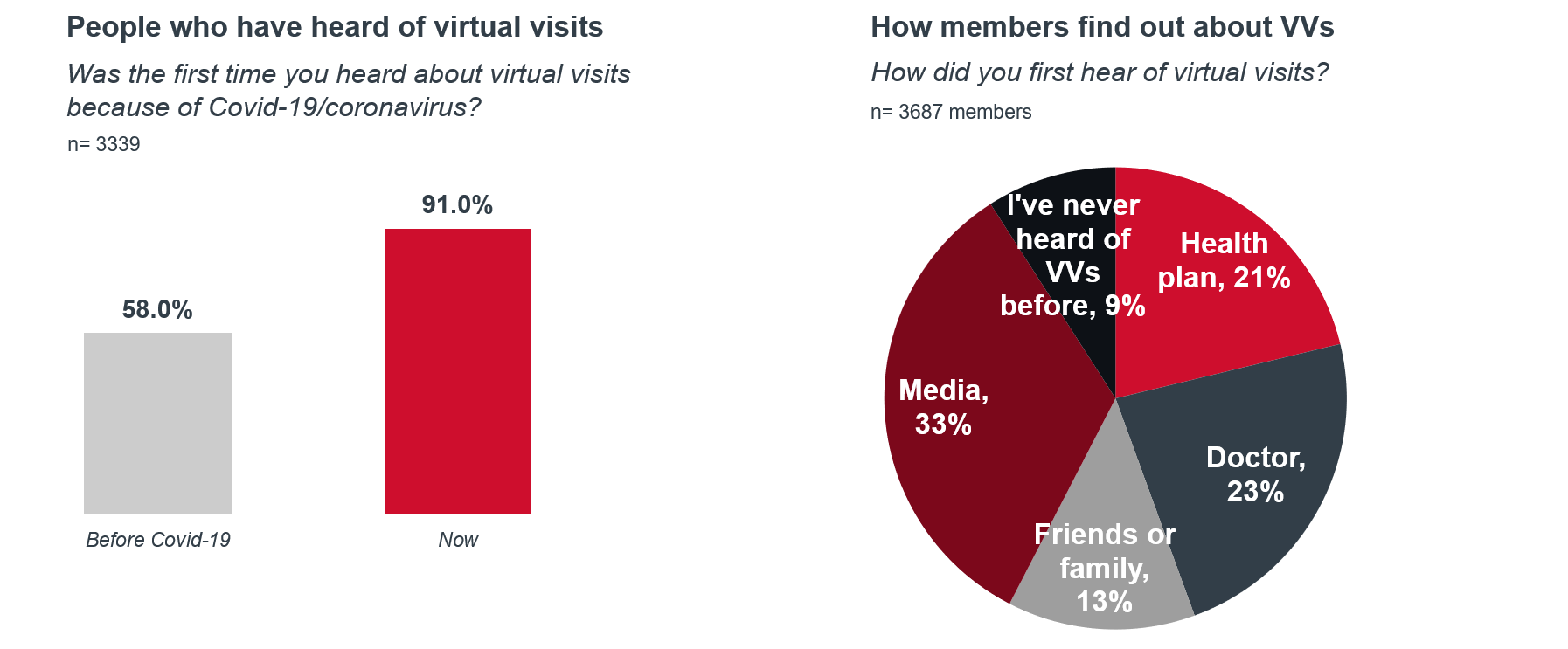
2. Learn from past mistakes: Health plans were too slow with their messaging about virtual visits.
While more consumers than ever utilized virtual visits in 2020, most of them don’t give their health plan credit for that introduction. Health plans spent a significant amount of resources aimed at communicating their virtual visit offerings to members, but they came up short. Most survey respondents reported having first found out about virtual visits through the media, followed by their doctor. Read our article here for examples of plans that communicated well with members immediately about Covid-19.
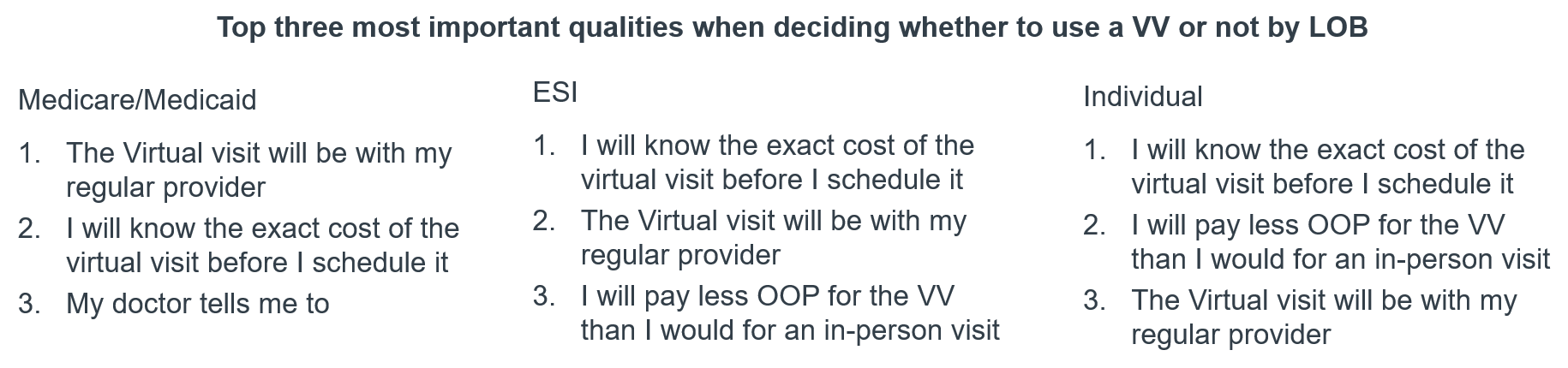
3. What’s more important: Provider continuity or cost transparency? It depends on the LOB.
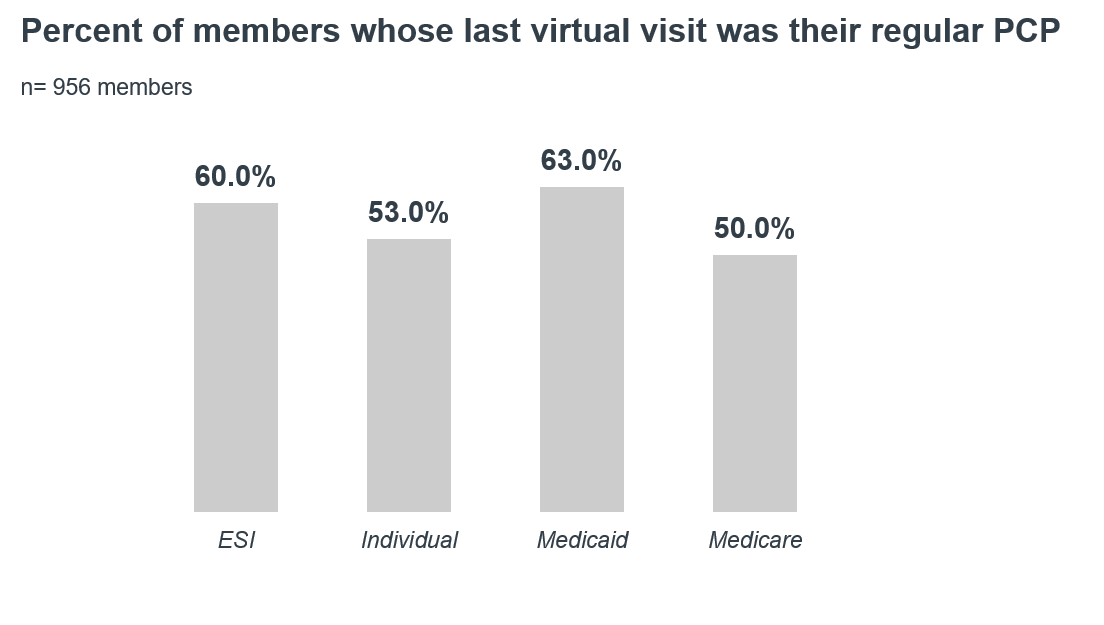
As payers shift their virtual visit strategy from a reactive pandemic response to a sustainable long-term site of care, it's important to consider what their members want from these types of visits—and that those qualities are not one size fits all. Medicaid and Medicare Advantage members ranked provider continuity as their most important quality when deciding to use a virtual visit. Currently, although Medicaid members were the most likely to have had their last virtual visit with their regular PCP (at 63%), Medicare Advantage members were the least likely (at 50%). On the other hand, those on employer sponsored insurance (ESI) and individual market members valued knowing the exact cost of the visit before scheduling as their top quality. It is important to note that their top choice was cost transparency not lower costs.
Questions to consider as you plan your organization’s future strategy
Virtual visits are here to stay—the level at which they stay, will greatly be influenced by how health plans integrate consumer preferences in the design and marketing of their offerings. The following are questions to consider as health plan leaders evolve their virtual visit marketing strategy:
- Who are we missing in our virtual visit marketing? Is it equitable?
- What types of visits do we want to encourage members to use? Is that clear?
- What types of partnerships can help amplify our message?
Next, read about how telehealth is transforming how we think about clinical guidelines, track outcomes, manage patient hand-offs, and determine which care happens in which settings in our article, Five ripple effects of increased telehealth adoption
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.

