Auto logout in seconds.
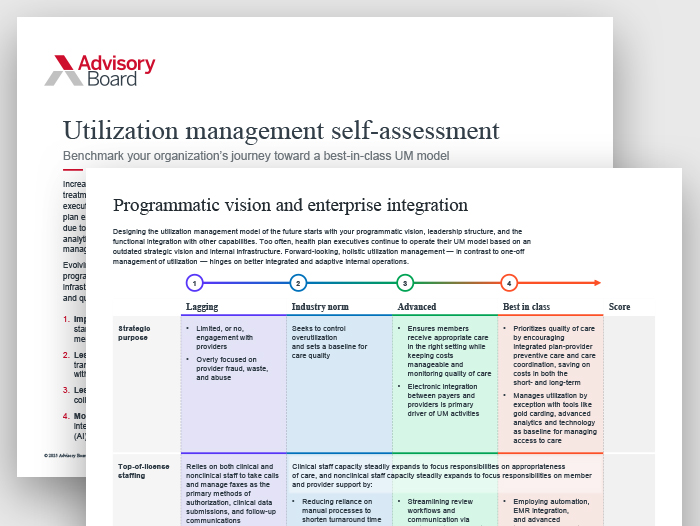
Continue LogoutHealth plan executives struggle to realize more effective utilization management programs due to pervasive abrasions throughout the process, lack of comprehensive data analytics, and an overreliance on one-size-fits-all policies rather than holistic management of utilization across a member’s care journey. Evolving utilization management requires plans to mature across four key domains: programmatic vision and enterprise integration; data exchange and technology infrastructure; program execution; and performance on access, outcomes, cost, and quality.
Programmatically, the future of utilization management is:
- Impact-driven, focusing UM activities only where there is proven value, balancing standardization and adaptability across unique plan-provider relationships and member needs.
- Less reliant on prior authorization as its main lever — via increased transparency of UM requirements, criteria, and outcomes — and better integration with both plan and provider care management.
- Less abrasive for providers and consumers as a result of increased collaboration with, and integration between, plans and providers.
- More efficient and less resource intensive for plans through bi-directional data integration and the adoption of advanced technology such as artificial intelligence (AI) and machine learning.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.