Auto logout in seconds.
Continue LogoutPhysicians report that they or their staff spend 16.4 hours per week completing preauthorization requests—that’s two days out of a five-day work week.
But plans must use preauthorizations to help keep premiums and deductibles affordable for members, so many plans feel forced to weigh cost management and provider satisfaction goals against one another.
However, these don’t have to be contradictory—plans can modify the preauthorization process to accomplish both goals.
Change the Messenger—Not the Message
To make progress on both objectives, plans must recognize that they’re not the best messenger. Providers, trained in clinical care, are frustrated by the perceived results of preauthorizations—either an approval that they find unnecessary, or a denial that seemingly disrespects their clinical judgment.
Instead, plans can turn to other trusted clinical experts to communicate utilization requirements and make preauthorizations more palatable. Read on for three experts that plans can deploy as messengers for a provider-centric preauthorizations process.
Messenger 1: Clinical Organizations
Highmark, a Blues plan based in Pittsburgh, completely removed preauthorizations—as long as providers followed standard clinical guidelines.
Highmark informs their providers in their clinical oncology pathways program that the clinical treatment pathways are set by the National Comprehensive Cancer Network (NCCN), a nonprofit third-party alliance of cancer centers. Participating providers are required to adhere 80% of the time to part B drugs that are part the standardized pathways. And as long as providers follow the pathway, they get preauthorizations waived for 40 chemotherapy drugs.
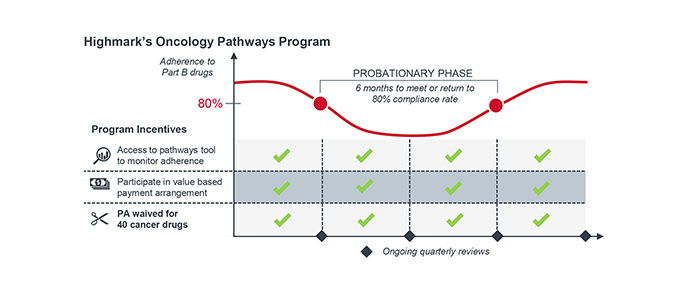
Highmark has seen a 10% reduction in medical spend across the 30 participating practices, and both providers and patients are happier because treatments can start 36-48 hours earlier.
Messenger 2: Familiar Specialists
L.A. Care, a Medicaid plan in California, automatically approves preauthorizations for specialty referrals—as long as the PCP gets a second opinion from an in-network specialist.
The PCP has to use L.A. Care’s online messaging platform to ask the specialist if the specialist visit is warranted, and if so, what labs or tests the specialist would want in advance. The eConsult tool allows the PCP to search through all in-network specialists and securely send patient details to the specialist of the PCP’s choice.
This process still guarantees that PCPs are only making necessary specialist referrals, but PCPs no longer have to deal with tedious authorization requests. Instead, a fellow provider serves as the approver—and can give clinically sound alternatives when no referral is necessary.
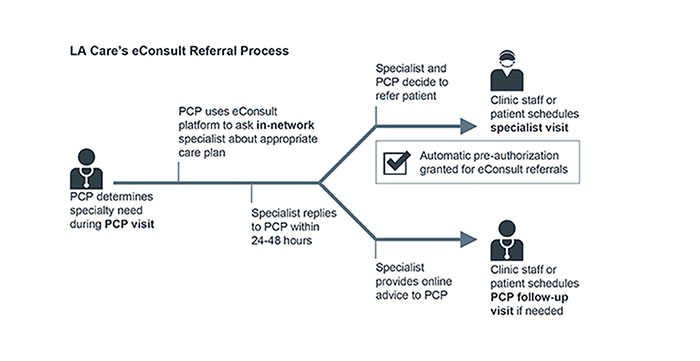
L.A. County Department of Health Services also implemented a similar portal and saw 150K consults and a 25-48% decrease in number of specialist visits.
Messenger 3: Physician Peers
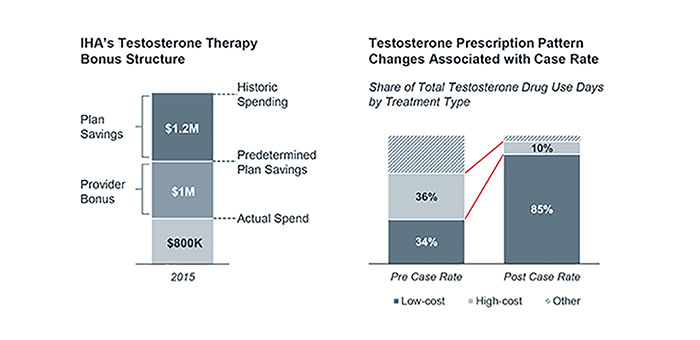
Independent Health Plan (IHA), a large plan in western New York, delegated preauthorization to a provider practice—but only after supplying them with cost information for a drug class with wide cost variation.
The participating urology practice, also involved in one of IHA’s value-based payment programs, was surprised to see IHA’s data on the wide variation in price for different testosterone drugs. After the plan highlighted the potential savings opportunity, the provider practice’s steering committee drafted new prescribing protocols for their physicians and the reimbursement model around them.
In the first year of the program, providers saved IHA $1.2 million dollars and earned $1 million in savings. The provider practice designed the restrictions and benefited from the savings.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.


