Key Takeaways
- Digital inequity, also known as the digital divide, refers to the economic, educational, and sociocultural disparities that arise from inadequate access to and utilization of technology.
- Lack of access to technology is a social determinant of health.
- Telehealth’s rapid scaling during Covid-19 has exacerbated access disparities, making the digital divide even more pronounced among vulnerable populations.
- Providers’ new investments in technology and telehealth will worsen these inequities if there is no action, harming the patient populations who could benefit from them the most.
Digital inequity, also known as the digital divide, refers to the economic, educational, and sociocultural disparities that arise from inadequate access to and utilization of technology. Without access to technology, disparities in education, employment, housing, and health care worsen, leading to a cyclical pattern of inequality. Technology access also impacts the type and quality of care patients are able to receive, especially as more care is delivered via technology such as telehealth platforms.
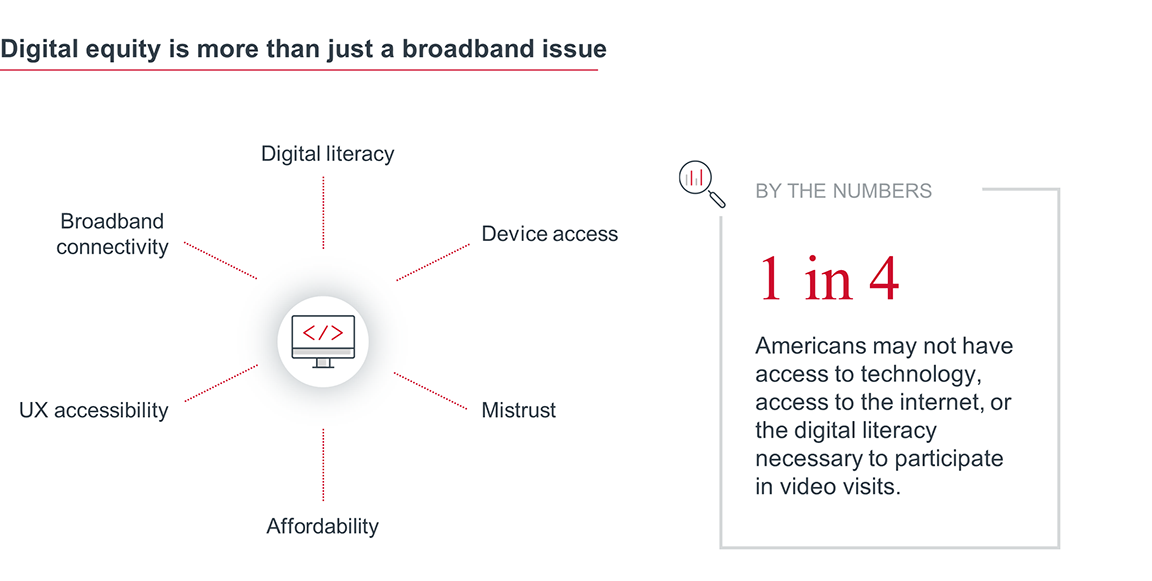
Barriers in access to digital health platforms include poor digital literacy, disabilities, lower income, and limited English proficiency. Larger, structural challenges to the digital divide include geographic isolation, broadband capacity, and lack of technical hardware needed for virtual health care access.
Advisory Board believes that lack of access to technology is a social determinant of health that has widespread ramifications across education, employment, and health care. Failure to address these inequities will exacerbate disparities across the care continuum and widen the digital divide.
The Covid-19 pandemic heightened interest in digital tools because of their scalability, efficiency, and portability—and growth in this space continues. This past year saw a record $14.8 billion raised in equity for digital health funding, and digital transformation is the top strategic priority cited by CFOs for 2021.
This industry-wide emphasis on digital tools is beneficial for patient monitoring and care delivery, but it also necessitates a second look at how these advancements could help—or harm—existing digital inequities among disconnected populations. Left unaddressed, the digital divide will embed a two-tiered system of care based on technological access. Affluent patients will have a full-spectrum of care options, while disadvantaged individuals will be forced to rely on in-person visits or substandard workarounds.
The mandate here is clear: investments in digital health are critical, but providers must factor in equity at the outset. Lack of action will harm the patient populations who could benefit from digitally enabled care the most.
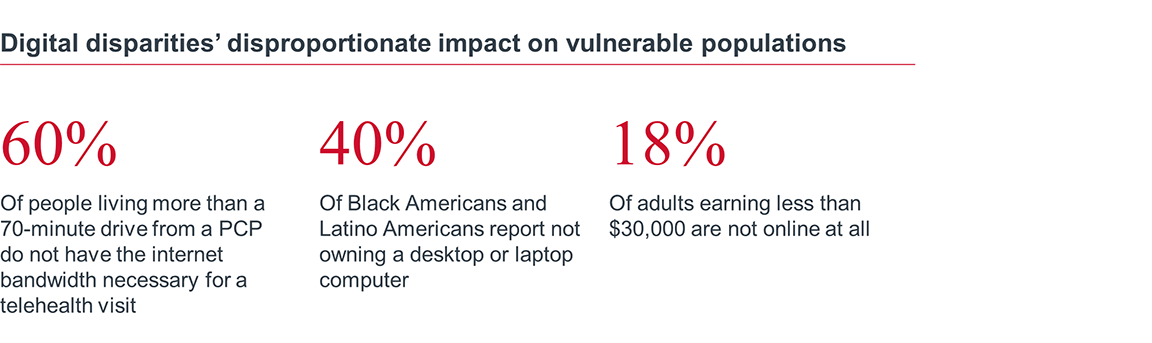
Obvious contributors to digital inequity include broadband connectivity, device access, and digital literacy. However, these are only the outermost layers of a deeper problem. The root of digital disparities is tied to the systemic educational, employment, and socioeconomic disparities among disadvantaged populations across the country.
Inequity is a cyclical issue. Inadequate education limits employment opportunities, which exacerbate disparities in housing, nutrition, and safety. Parallel to these inequities is a widening gap in technology access and digital literacy. This results in disadvantaged individuals who are also disconnected from important technological touchpoints, such as health care. As more care delivery shifts to the virtual setting, digital inequities will worsen health outcomes related to technology, as well as the existing cycle of other social determinants of health.
Digital inequity is a multipronged issue and demands a complex response. Here, one thing is clear: no single stakeholder is responsible—or capable—of addressing it alone. Providers, payers, vendors, and policy leaders must work in tandem to first understand the needs of disadvantaged and disconnected patients and then identify solutions to bridge the divide.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.

