Auto logout in seconds.
Continue LogoutHHS' recent approval of Kentucky's Medicaid work requirement waiver is shining light "the relationship between oral health and work"—and the negative health and economic implications for Medicaid beneficiaries who lack dental coverage, Austin Frakt writes for the New York Times' "The Upshot."
Learn more: Get profiles of state-level Medicaid transformation
The state of US dental coverage
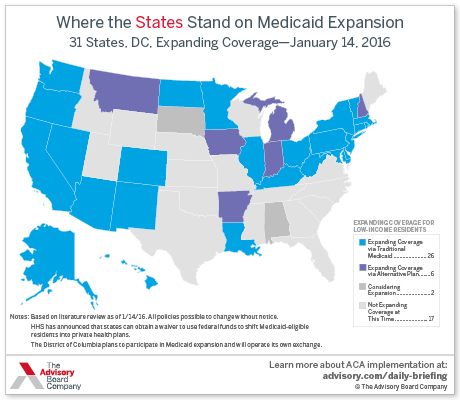
While state Medicaid programs are required to cover dental care for eligible children, the programs are not required to cover such services for low-income adults. As a result, Frakt writes most states offer "limited dental benefits or none," and just 17 state Medicaid programs offer comprehensive dental benefits for low-income adults. Of those, 14 offer dental coverage to the population eligible for Medicaid under the Affordable Care Act (ACA).
Frakt acknowledges that most private health care plans also lack comprehensive dental coverage, but argues that the Medicaid-eligible population is much less likely to be able to afford dental care than those who are enrolled in private health plans through their employer, and as a result more likely to need those services.
The link between poor dental care and poor health
Frakt cites research demonstrating that poor dental health is linked to a large number of other issues. Periodontal disease, for example, is linked to an increased risk of both cancer and cardiovascular diseases, while bacteria from oral infections can contribute to heart disease and strokes. In addition, studies have shown that pregnant women who lack dental care have an increased risk of preterm delivery, Frakt writes.
Poor oral health also can lead to tooth pain or tooth loss, which Frakt writes can limit the types of food people can eat, resulting in potentially unhealthy dietary changes.
Sidney Whitman, a dentist from New Jersey who treats Medicaid beneficiaries, told Frakt that he has seen the consequences of poor oral health in his own practice. "Without adequate oral health care, patients are far more likely to have medical issues down the road," Whitman said.
The link between poor dental care and employment
The consequences of poor oral care extend beyond one's health, Frakt writes, citing research that has shown it also can affect the "ability to find and keep a job."
However, Frakt writes that several states considering Medicaid work requirements do not offer comprehensive dental benefits. For instance, Frakt writes, " Arkansas, Indiana, and Kansas offer limited benefits"; "Maine, New Hampshire, and Utah offer emergency-only benefits"; and "Arizona offers none."
In Kentucky, Frakt notes Medicaid beneficiaries—including those who will be subject to the state's newly approved work requirements—have access to "limited dental benefits." He explains, "Those benefits exclude coverage for dentures, root canals, and crowns, which could challenge some enrollees' ability to maintain good oral health and lead to greater emergency department use."
So what can be done?
At the very least, Frakt writes states should offer emergency dental care through Medicaid. He cites a study based on Oregon's Medicaid expansion that found emergency dental coverage led to more people receiving dental care, "largely through emergency department use."
Frakt concludes, "It's an accident of history that oral care has been divided from care for the rest of our bodies. But it seems less of an accident that the current system hurts those who need it most" (Frakt, New York Times, "The Upshot," 2/19).
March 7 webconference: Learn the key health care trends to watch for in 2018
Join us next Wednesday at 3 pm ET to learn about the most important forces shaping the health care industry in 2018--including payment reform, policy changes, consumer purchasing decisions, new service sites, and more.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.