Auto logout in seconds.
Continue LogoutKey Takeaways
- Health disparities at the point of care occur when different demographic groups experience inequitable treatment while interacting with health care systems, care teams, and staff.
- Health disparities at the point of care can negatively impact clinical outcomes, patient safety, length of stay, readmissions, and the patient experience.
- Health disparities at the point of care have far-reaching consequences for patients, but also for health systems’ business priorities. Health systems must ensure inclusive and effective care for all groups within their community to remain successful.
Health disparities are differences in illness, injury, disability, or mortality rates across population groups. Certain population groups experience poorer health outcomes and health care services relative to other groups, even after accounting for variations in health care needs, patient preferences, insurance status, and recommended treatments.
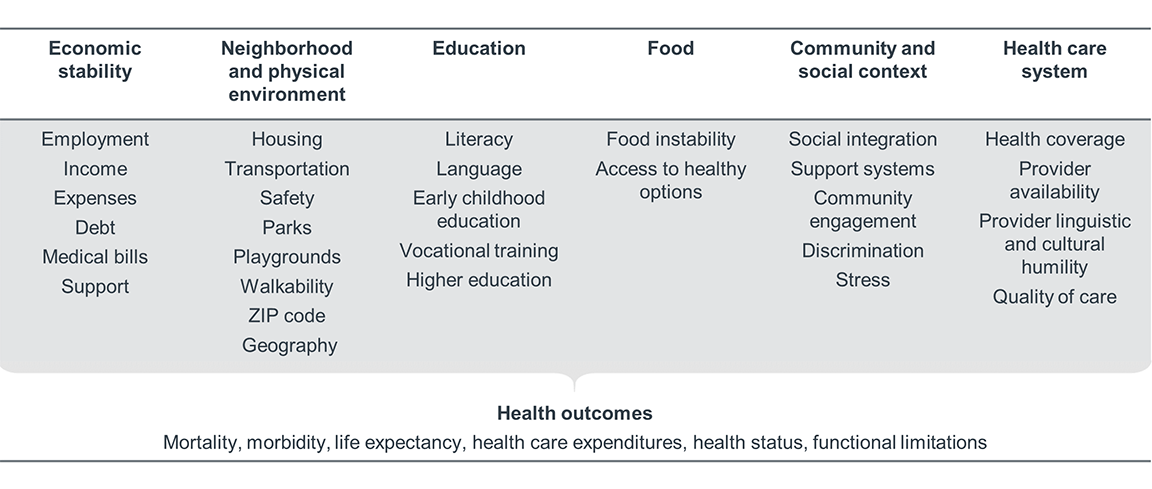
Health disparities are the result of more than individual, interpersonal, or biological factors. They are driven by complex interactions between many factors relating to individuals, clinicians, health care systems, environments, communities, and society.
Health disparities at the point of care occur when different demographic groups experience inequitable treatment while interacting with health systems, care teams, and staff. This inequitable treatment can negatively impact clinical outcomes, patient safety, length of stay, readmissions, and the patient experience.
Disparities in care delivery are often caused by the patient-provider interactions and other health care system-level factors listed in the rightmost column of the table above. Disparities at the point of care can result from an insufficient understanding of patient needs, to bias and discrimination from the level of the entire health care industry to the individual provider level.
Historically, health care has been unequally allocated among demographic groups. And despite changes in policy and public sentiment, this historical legacy continues to negatively influence the modern health care industry and perpetuates inequitable care delivery.
While most clinicians are committed to treating patients equally, they still operate within a society and health care industry that is inherently biased and unjust. Clinicians, like the rest of the general population, hold explicit and implicit biases. Clinicians’ implicit biases, or their unconscious attitudes and stereotypes about groups of people, can easily affect the way they treat patients. These unconscious views can lead clinicians to make unintentional judgments and ultimately contribute to unequal treatment and worse health outcomes for certain patient populations.
Ample evidence indicates that disparities in care delivery and outcomes persist at the point of care. The examples below demonstrate the disparities at the point of care that occur along one or several demographic characteristics such as race, ethnicity, gender identity and sexual orientation, age, and language (REGAL).
Race/ethnicity
- Black patients and American Indians/Alaska Native patients received worse care than white patients for about 40% of quality measures.
- Hispanic patients received worse care than non-Hispanic white patients for about 35% of quality measures.
- Asian and Native Hawaiian/Pacific Islander patients received worse care than white patients for about 30% of quality measures.
- When cared for by white physicians, Black newborns are 3x more likely to die in the hospital than white newborns.
- Black patients reporting pain are 22% less likely than white patients to get pain medication from their doctors.
- 20% of Black adults report being treated unfairly based on their race while getting health care for themselves or a family member in the past 12 months.
- Black patients experience 9% longer ED waiting times.
- Black patients have a 9% longer postoperative LOS following elective
colorectal surgery even if no postoperative complications occur. - Black patients are 7% less likely to receive an urgent Emergency Severity Index score than white patients. Black patients were also 10% less likely than white patients to be admitted to the hospital.
Gender identity/sexual orientation
- Women in one urban emergency room wait an average of 16 minutes longer than men to get medication when reporting abdominal pain and are less likely to receive it.
- 25% of women experience a medical error in their lifetime, compared with 17% of men.
- Women are 50% more likely to be misdiagnosed following a heart attack.
- Women are 25% more likely to be misdiagnosed after a stroke.
- 70% of transgender or gender non-conforming patients surveyed have experienced some type of discrimination in health care.
- 56% of lesbian, gay, or bisexual patients surveyed have experienced some type of discrimination in health care.
- 52% of transgender respondents reported that they believed they would be refused medical services because of gender identity.
- 73% of transgender respondents reported that they believed they would be treated differently by medical personnel because of their gender identity.
- 29% of lesbian, gay, and bisexual respondents reported that they believed they would be treated differently by medical personnel because of their sexual orientation.
Age
- Vulnerable elderly patients receive about 50% of the care recommended by their providers.
- 1 in 5 adults over 50 experiences age-related discrimination in health care settings.
Language
- Limited English proficiency (LEP) patients are 25% less likely to receive full documentation of informed consent before undergoing invasive procedures.
- Hospitalized children of LEP parents are 2x more likely to experience medical errors than children of parents who expressed comfort with English.
- 49.1% of LEP patients’ adverse events involve physical harm.
- Patients who do not receive professional interpretation services at admission or discharge have an increase in their LOS of up to 1.47 days.
- Only 52% of non-English-speaking patients are satisfied with their care in the ED.
- 78.9% of Asian LEP patients do not have access to language assistance at their usual source of care.
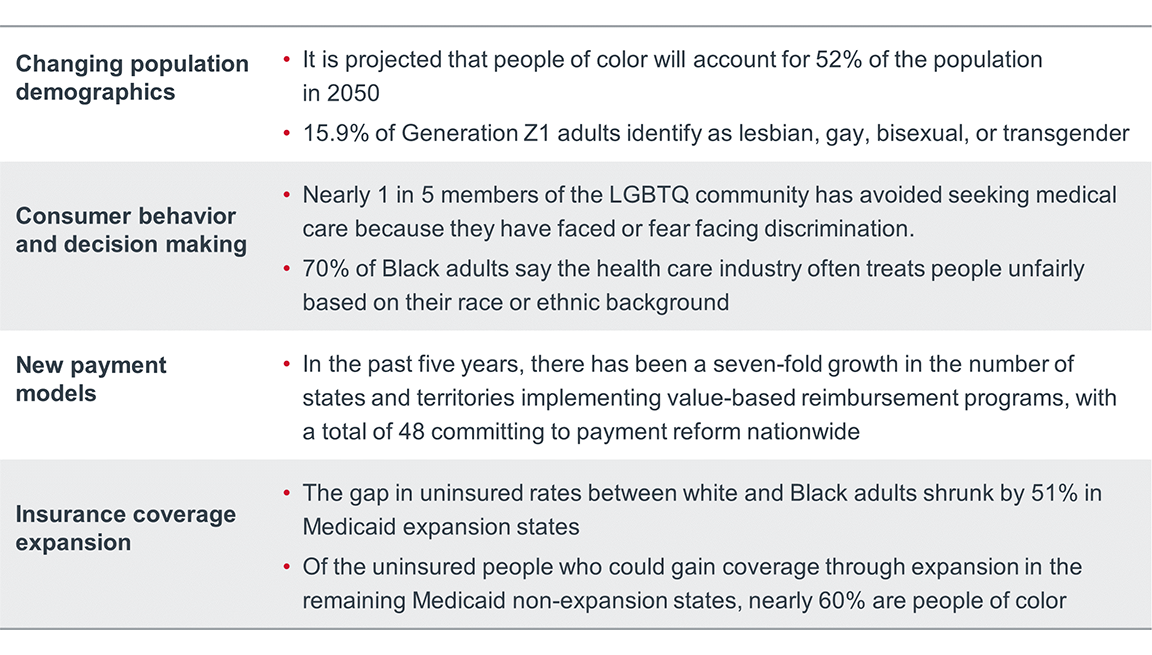
Disparities at the point of care have far-reaching consequences for patients, as well as for health systems’ business priorities. As payment models increasingly incorporate patient experience and quality of care, disparities in care delivery will negatively impact provider organizations’ bottom lines. In addition, the discrimination patients experience within health care settings can influence their future behavior. Patients may avoid seeking care as a result of discrimination they have experienced or anticipate they will experience. Simultaneously, minority populations are growing, and their access to health care is expanding. Health systems must ensure inclusive and effective care for all groups within their community to remain successful.
Health systems are often unaware of differences in the care experiences and health outcomes of their patients, and they frequently do not account for patient social needs that may be driving those differences. The framework below provides guidance on how health systems can develop a strategy for detecting and addressing disparities among their patients.
Educate leadership
• Educate leaders about the prevalence and impacts of health disparities, at the pointof care and more broadly at the population level.• Get leadership buy-in to focus on reducing disparities for your workforce, patients,and community.
Assess current disparities
• Develop a data-collection strategy with the ability to stratify clinical outcomes andprocess-of-care metrics by REGAL demographic data at a minimum.
Analyze impacts
• Detect major patterns of disparities in care.• Analyze impact of disparities on the community.• Take an intersectional approach to data analysis to identify groups most at risk ofexperiencing inequities.
Identify potential causes
• Investigate high-impact disparities to identify underlying root causes and drivers.• Use qualitative data sources to add context to patterns in quantitative data.
Target interventions
• Develop interventions aimed at addressing the specific drivers and root causes ofmajor disparities.• Uplift and center community perspectives to build effective, sustainable interventions.
Monitor performance
• Establish formal methodology for evaluating interventions’ impact on reducing healthdisparities at the point of care.• Assign clear accountability for program improvement responsibilities.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.

