Auto logout in seconds.
Continue LogoutDoctors and nurses want to be with patients. They want to be caregivers. The problem is that they are tasked with too many other things that make it difficult for them to work at top of license.
Top of license work has long been an aspiration of our clinical workforce. We want all of our clinicians’ education, training, and expertise to be put to use. We want to steer their work and workflows away from things where all of that training and expertise doesn’t add any value.
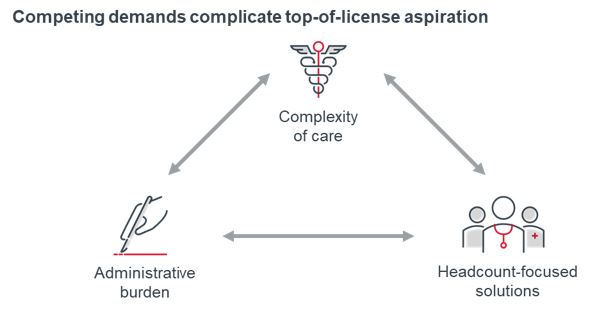
Advisory Board’s research on top-of-license work for nurses and care teams across the past decade has consistently said the same thing: there are competing and consistently escalating demands on clinicians that make it hard to practice at top of license. The reality is that we need clinicians practicing at top of license because care complexity continues to increase in terms of the number of conditions, comorbidities, medications, and providers a patient has.
"Fatigue rarely comes from the specific thing people are supposed to be or want to be doing, like patient care. It comes from all of the additional [things] we ask them to do, typically administrative, not top-of-license stuff."
At the same time, the administrative burden on clinicians is enormous. “Too many bureaucratic tasks” is the top contributor to clinician burnout: nearly three out of five physicians say it is the biggest contributor to their feelings of burnout. That’s not a surprise: between one-third and one-half of physicians’ time is spent reviewing medical records and writing notes.
Unfortunately, most health care organizations see hiring more staff as the only way to address the complexity of care and to relieve the administrative burden. The reality of provider finances and labor markets is that they can’t add staff—they can’t afford it, or qualified candidates aren’t available, respectively. Nine out of every 10 nurses say that they have considered leaving the nursing workforce, mostly because of staffing constraints.
Advisory Board has literally written the book on care-team redesign, and that undertaking is an important step in understanding and advancing top-of-license practice. But given the increasing complexity of the issue, it’s not unreasonable to think that health care has reached a point where clinicians simply can’t practice at top of license without a new approach to the problem.
Artificial intelligence excels at repetitive tasks that humans usually perform as the connective tissue between silos of data and accountability. The solutions available incorporate many different kinds of technology — voice recognition, predictive classifiers, natural language processing, and computer vision are relatively common — which can then be layered on top of robotic process automation to create adaptive and resilient applications. These solutions can do repetitive tasks, but they can also learn and be taught to do them differently and better as needs change.
There’s a pervasive misconception in health care that any implementation of AI is effectively handing over processes to an unaccountable, inscrutable bot that will ignore outliers and boss clinicians and staff around. We’d never hire a person like that, so why would we hire a computer to be that way?
A clear understanding of both AI’s potential and its limitations can help health care leaders think about its uses in ways that will drive results. Health care has begun to embrace AI across the care enterprise to make business processes like revenue cycle and human resources more efficient. Those are worthy and necessary investments. But they do not help address the fundamental risk to both mission and margin that clinician burnout poses.
Artificial intelligence or automation — of any kind — in clinical care can be a sensitive subject. Neither providers nor patients want to lose the human connection of delivering and receiving care. The reality is that health care must deploy these technologies because, if for no other reason, clinicians are tired and must have more robust support.
Scroll down below to discover the three ways AI is already working to enable top-of-license practice:
- Help clinicians add value to patient interactions.
- Reduce clinical documentation demands.
- Make accountability more than just scolding clinicians into compliance
Top of license
To practice to the full-extent of one’s education and training — making the greatest contribution each individual can make — rather than spending time doing non-value-added work.
Artificial intelligence
AI is a broad term, representing our intent to build humanlike intelligent entities for selected tasks. The goal is to use fields of science, mathematics and technology to mimic or replicate human intelligence with machines.
AI comprises components such as machine learning, neural networks, computer vision, natural language processing, sensors, human-AI interactions, planning and reasoning, and autonomy. 1
Intelligent automation
AI-enabled process automation.
Intelligent automation combines adaptive elements of AI like predictive classifiers, natural language processing, and computer vision with execution-focused capabilities of RPA to perform repetitive, logic-based tasks.
It uses AI capabilities to take in and act on structured and unstructured data in a human-like manner and learns from historic data to improve accuracy and efficiency.
Clinicians value time spent caring for their patients but in reality, a large portion of their time with patients is spent searching for the right information in the EHR. The problem for frontline clinicians is not a lack of data. It’s too much data. The challenge is separating the vital few from the trivial many.
In conversations with clinicians who are using AI-enabled solutions, we have heard two consistent themes about what those systems allow clinicians to do.
"You came in to talk about cancer. So why would we spend time together talking about your history of allergies?"
Any time during the clinical visit that is spent talking about something other than the issue at hand is frustrating for the clinician and the patient. Automated pre-visit and intake solutions, enabled with AI to be adaptive to what the patient reports, can also cue up the relevant information to the clinician, without requiring the clinician to do the “librarian” work of gathering, collecting, and summarizing information.
"I can be more productive and more focused on the patient."
Even and especially for high-performing, high-productivity physicians, AI-enabled solutions can support them to add value to patient interactions that is truly unique to them. Their experience, expertise, and time is wasted if they are wading through screens in the EHR. From a throughput perspective alone, less time spent on documentation means more time with attention on patients—and potentially more patients.
Notice that none of this relies on an idealized end-to-end technology that replaces the primacy of the clinician’s expertise and judgment in the patient interaction. Just because AI can be deployed autonomously to complete a repetitive task over and over, that doesn’t mean AI has autonomy to act on its own. The power of these technologies is to liberate clinicians to do the patient-facing work they want to do, rather than the non-value-add work that they often have to do.
The amount of time clinicians spend on documentation as part of their workday is a genuine time sink that contributes significantly to burnout. In 2013, Advisory Board researchers wrote about helping nurses practice at top-of-license, and the very first element of those recommendations was to streamline documentation demands. Nearly a decade later, the demands have only increased, both in terms of volume and complexity.
AI-enabled solutions can reduce the data that clinicians are responsible for collecting at the point of care and entering into the medical record. Voice transcription and scribing are increasingly prevalent and accurate. Newer asynchronous questionnaires employ branched logic to suggest triage and diagnosis while automatically populating the relevant fields in the medical record and writing the visit note. Real-time ambient technologies are available to transcribe the entirety of a patient-clinician interaction.
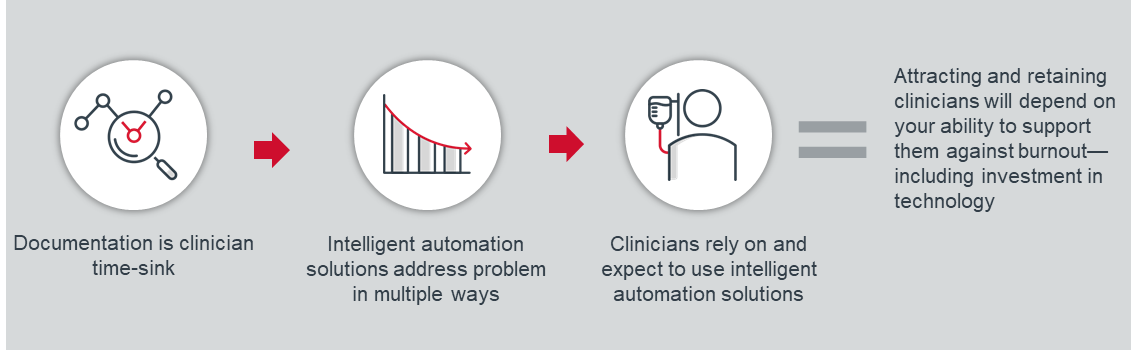
But the insight about these technologies is not that there is a documentation problem and that technology can reduce or eliminate it. The insight is about what happens as these technologies get better and cheaper. The answer: more clinicians will use them, and indeed begin to rely on them as a regular part of their practice.
Attracting and retaining clinicians in the future is going to depend heavily on how any health care organization supports them to deal with burnout — and part of that is going to be the technology that is provided to make their work easier. Clinicians will choose to work where automation allows them to spend more time on patient care, rather than documentation. They won’t be willing to spend hours after work and over the weekend to complete documentation when automation technology can do all that work for them.
Even if systems can automate away many administrative tasks, clinicians will still bear the burden of completing some tasks for which they personally have few incentives but are important to the health system or other stakeholders. There’s always someone who wants a clinician to complete another report or plan.
While AI can provide automated visibility into how well clinicians adhere to those processes, the opportunity isn’t in monitoring clinicians in a far more pervasive if accurate way. It’s not even in being able to send them more specific or robust alerts to scold clinicians into compliance. It can be about identifying high performers and learning from them.

We’ve seen systems that are designed to identify and automate clinical processes and reporting for things like discharge planning and scheduling, and even to prompt intervention from a clinician or staff member when appropriate. But we can also use this technology to close the accountability loop, not only by picking out adverse actions and outcomes for attention and escalation but also by identifying actions and outcomes that should be reinforced with recognition. Leaders can use this information to give high-performing clinicians kudos for a job well done. That’s solving a problem of clinician experience that goes far beyond simply helping them spend less time on a tedious task.
Again, clinicians can be sensitive to AI of any kind in the clinical care setting. Too many clinicians think that AI and automation will make their jobs worse — either by introducing a clunky solution that requires more work on their part or by creating a workflow that replaces human touch with a digital solution. And without clinician support, any attempts to deploy these technologies will be unsuccessful. As you start to invest in and deploy these solutions, it’s important to remind clinicians that the ultimate goal is to help them do their jobs better and to make their work more enjoyable.
Bright.md is a leading virtual care solution trusted by health systems to automate clinical workflows and administrative tasks, improving patient and provider engagement and driving operational efficiency. With its pioneering technology, Bright.md improves how health systems deliver care, from patient acquisition through clinical interview and treatment, to reduce 90% of administrative workflows, lower patient wait-times to 6 minutes on average, and drive patient loyalty with industry-leading satisfaction ratings.
This research was sponsored by Bright.md. The content, views, and opinions contained herein are copyrighted by Advisory Board and all rights are reserved. Advisory Board experts wrote the content, conducting the underlying research independently and objectively. Advisory Board does not endorse any company, organization, product or brand mentioned herein.
[1] Holley K and Becker S, AI-First Healthcare: AI Applications in the Business and Clinical Management of Health, O’Reilly Media, 2021.
This article is sponsored by Bright.md. Advisory Board experts wrote the article, conducting the underlying research independently and objectively. Bright.md had the opportunity to review the article.
Learn MoreDon't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.

