Auto logout in seconds.
Continue LogoutAfter months of procedure delays, many cardiovascular (CV) administrative and physician leaders are beginning to relaunch elective services at their hospitals and health systems. But determining when it's safe to resume elective services is only half the equation; leaders still must determine how to resume these procedures—including which procedures to rollout first, how to balance the backlog of postponed cases with emerging demand, and overall supply, labor, and capacity constraints.
To help, we outline why CV service line leaders should prioritize electrophysiology (EP) procedures as they navigate our "new normal," based on our three-part framework of considerations—clinical urgency, financial and strategic importance, and overall procedure feasibility.
Click here to download this blog post in PDF format
1. EP procedures are clinically urgent
Health system leaders should prioritize treating CV patients because of the clinical nature and progression of cardiovascular disease (CVD) and the substantial risk of adverse outcomes. Based on the acuity level of CV patients, elective CV procedures are typically more urgent than elective procedures in other service lines, such as cosmetic or orthopedic procedures, since appropriate CV interventions can delay disease progression. Elective EP procedures, in particular, can treat patients with potentially dangerous cardiac arrhythmias; these procedures include catheter ablations, as well as device implants and left atrial appendage occlusions (LAAO).
Unfortunately, many CV patients have been delaying treatment at hospitals to avoid exposure to Covid-19, the disease caused by the new coronavirus. For instance, when Cigna reviewed claims data for its 14 million commercial members between March and April, the organization found hospitalization rates dropped 35% for atrial fibrillation (AF) and 31% for transient ischemic stroke (TIA)—declines far more significant than seen with other conditions. This is particularly concerning for AF patients given the high stroke risk and the fact that delayed treatment can worsen outcomes.
Given the substantial risks of cardiac arrhythmias, EP procedures—including catheter ablations—should be prioritized when tiering elective CV procedures.
2. EP procedures are financially beneficial—and strategically important
Next, health system leaders should evaluate the importance of each service for their systems' goals and priorities.
For instance, in terms of the financial implications, the CV service line is a growth engine for most hospitals—CV surgery ($3.70M) and invasive cardiology ($3.48M) have the highest net annual revenue compared to all other service lines. Within the CV service line, EP procedures garner favorable reimbursements for both Medicare fee-for-service and commercial patients. Case in point: median Medicare revenues-per-case are more than twice as high for inpatient EP services ($20,520) as they are for inpatient CV services as a whole ($9,600). 1 This includes median revenues of $23,240 for DRG 273 (ablations w/MCC) and $19,460 for DRG 274 (ablations w/o MCC) as of 2020. Commercial reimbursements are even more favorable, which is particularly important given the large portion of commercial patients receiving EP procedures; based on Premier data from 2019, the payer mix for ablations, as an example, was 51% Medicare, 39% commercial, and 5.6% Medicaid. Notably, median reimbursement for these commercial ablation cases ranged from $51,512 for DRG 274 up to $55,825 for DRG 273. Outpatient ablations, which we see increasingly among the younger, commercially insured population, garnered about $33,417 in reimbursement in 2019 as well. 2
Profit margins are equally favorable for EP procedures. In fact, the median inpatient Medicare profit per case for EP services is 60% higher than the median inpatient profit per case for all cardiac services. 3 And since commercial rates are significantly higher than Medicare rates, the median commercial profit for these procedures is significantly higher as well. For ablations, in particular, we see median commercial per-case profit margins of 54% for DRG 273 and 58% for DRG 274. 4
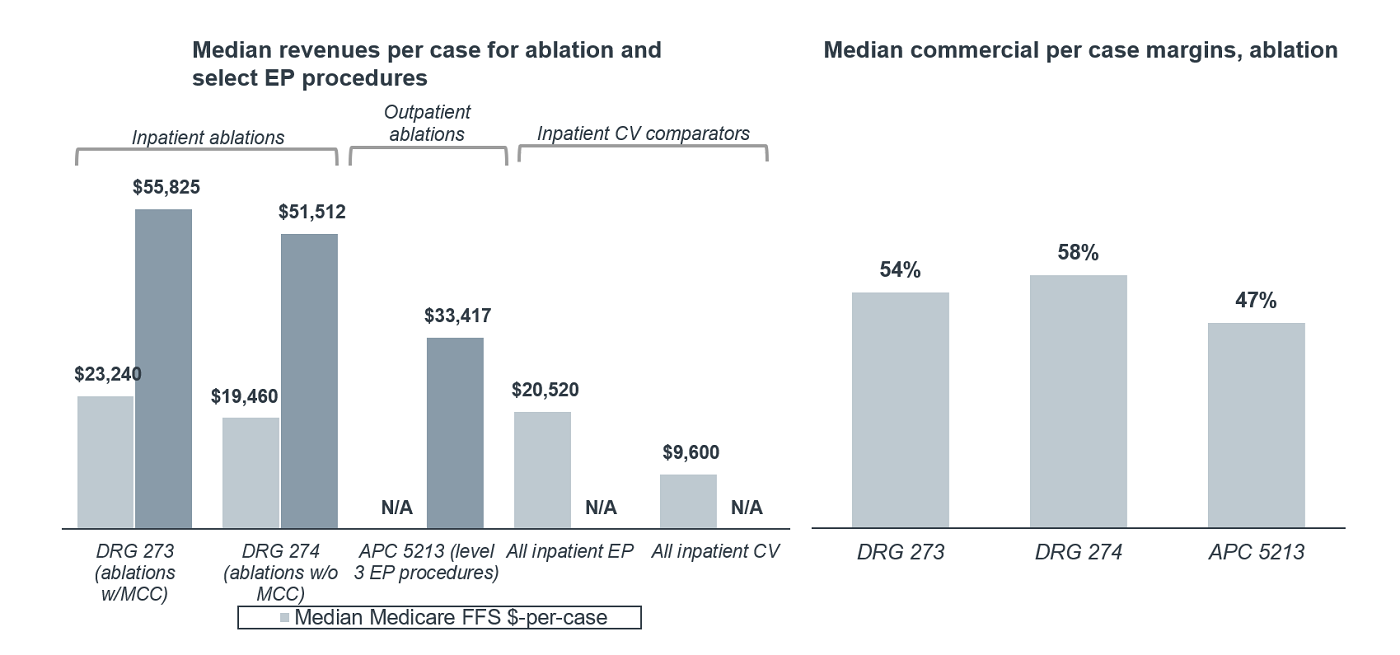
Outpatient EP services are also highly profitable for most health systems, even when compared to other cardiac services. In fact, the median outpatient Medicare profit per case for EP services is 319% higher than the median outpatient profit per case for cardiac services overall. 5 Using ablation again as an example, profit margins for commercially reimbursed outpatient cases are also quite healthy, with median profit margins for commercial ablation patients coming in at around 47% in 2019. 6 The favorable revenues and margins for these critical EP procedures can go a long way to help hospitals recoup profitable revenue lost during the early months of Covid-19.
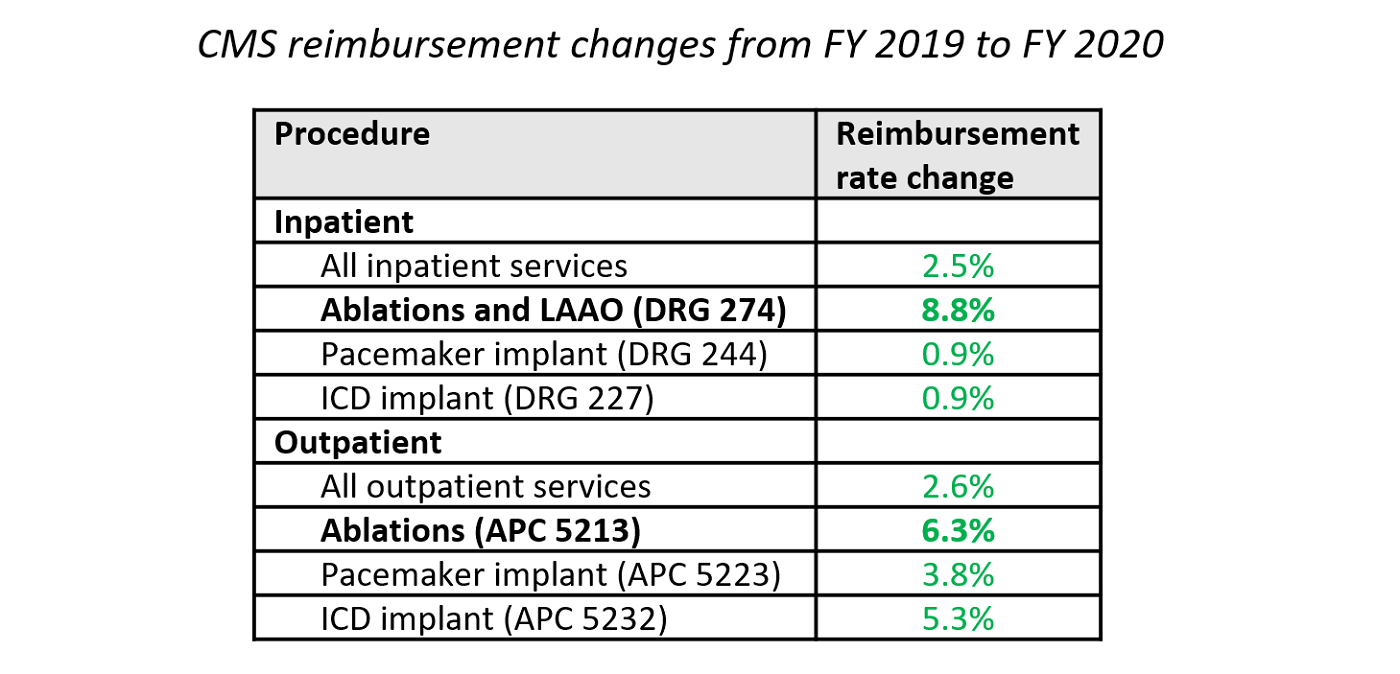
Beyond the short-term, EP will continue to be a strategic priority for CV service line moving forward. As evidence, Medicare reimbursement rates for many EP procedures have been growing over the past few years. Although reimbursement rate increases vary widely across the range of EP procedures, they have continued to increase across the board, with rate increases for ablations and LAAO far above average, as highlighted in the table below.
Beyond the financial aspect, many programs also view EP as a future growth opportunity. Given new and refined treatment options for AF patients in recent years, as well as a growing patient population, Advisory Board forecasts 18% growth in outpatient EP services by 2023. Understandably, competition has increased for this business—both from hospitals and ambulatory surgical centers (ASCs) that can provide EP services—which can provide enticing opportunities for EP physicians and teams.
As a result, CV leaders will want to ensure their EP care teams stay engaged in performing procedures at their system’s hospitals. Prioritizing ablations and other EP procedures in the queue is one sure way hospital leaders can show electrophysiologists how much they value their business.
3. EP procedures require less infrastructure relative to other procedures
After prioritizing services based on clinical urgency as well as strategic and financial performance, you must understand how you are going to perform these procedures. How feasibly can your program safely offer elective procedures, based on labor, capacity, and supply constraints, as well as personal protective equipment (PPE) and testing availability?
On the labor front, EPs should be readily available and eager to restart procedures; unlike other CV specialists, most EPs lack the necessary critical care background to be on the front lines treating Covid-19. And the staff support necessary for EP procedures is comparatively lower than it is in many other CV procedures, such as structural heart interventions—which means there will be less demand for staff PPE and testing. Additionally, EP labs have been going largely unused in the past few months, save for any emergent EP procedures, which means they are also readily available to ramp back up.
Moreover, in terms of capacity, EP procedures are often more efficient than other CV procedures, which will come in handy as programs balance their backlog of elective EP cases with normal demand. In fact, some programs are discharging EP device implant and ablation patients the same day they have their procedures—a move supported by new research in the Journal of the American College of Cardiology showing that same-day discharge for ablation is feasible for the majority of patients and is not associated with higher readmission rates or complications after discharge. And according to Premier data, 77% of ablations are already done on an outpatient basis, which means that more patients may be appropriate for same-day discharge compared with patients receiving inpatient ablations and other EP procedures.
Access pacemaker same-day discharge criteria in Optimizing Same-Day Discharge for CV Procedures
For programs still anticipating capacity constraints in the EP and cath labs, consider offering appropriate EP procedures off the hospital campus to free up lab capacity for higher-acuity cases, such as catheter ablations, left atrial appendage occlusion, and EP device implants for high-risk patients. For instance, CMS since 2018 has allowed insertable cardiac monitors, or implantable loop recorders, to be implanted in physician offices, and pacemaker and ICD implants can be performed in ASCs. (And even if your institution doesn't provide CV services in ASCs, certain procedures, such as pacemaker battery changes, can be offered in ASC settings with very little additional infrastructure.)
Looking ahead
As CV programs ramp back up elective procedures, prioritization of services will continue to be paramount for patients, providers, and hospitals. Due to the clinical urgency, financial and strategic importance, and feasibility of EP procedures, we believe EP services should be near the top of the list for CV leaders as they restart their elective programs. The months-long process will require ongoing monitoring of case mix and capacity, with the ultimate goal of balancing clinical urgency with feasibility.
This blog post is sponsored by Biosense Webster, Inc., a division of Johnson and Johnson and an Advisory Board member organization. Representatives of Biosense Webster, Inc. helped select the topics and issues addressed. Advisory Board experts wrote the post, maintained final editorial approval, and conducted the underlying research independently and objectively. Advisory Board does not endorse any company, organization, product or brand mentioned herein.
1. Average payment per case as reported in CMS' Inpatient Standard Analytical File (SAF); reflects Medicare fee-for-service discharges in 2018 Q4 - 2019 Q3. Claims involving outlier payments or non-Medicare primary payer codes have been excluded. This metric is not risk-adjusted. ^
2. Median commercial reimbursement figures for DRG 273, 274 and APC 5213 in 2019, sourced from IBM MarketScan data ^
3. Average contribution profit per case as estimated by The Advisory Board by subtracting direct cost from payment per case; reflects Medicare fee-for-service discharges in 2018 Q4 - 2019 Q3. Claims involving outlier payments or non-Medicare primary payer codes have been excluded. This metric is not risk-adjusted. ^
4. Per case profit margins estimated from median revenue per case (using IBM MarketScan 2019 commercial payer data) and median patient cost per case (using Premier 2019 all payer data). Per case profits reflect only direct patient costs and do not include fixed cost allocations. ^5. Average contribution profit per case as estimated by The Advisory Board by subtracting direct cost from payment per case; reflects Medicare fee-for-service outpatient encounters in 2018 Q4 - 2019 Q3. Encounters have been grouped by the most resource-intensive and/or clinically complex procedure they received according to the Advisory Board's outpatient grouping algorithm. Claims involving non-Medicare primary payer codes have been excluded. This metric is not risk-adjusted. ^
6. Estimates based on median revenue per case (from IBM MarketScan 2019 commercial payer data) and median patient cost per case (from Premier 2019 all payer data).^

Atrial fibrillation (AF) is one of the most challenging disease states for cardiovascular providers to manage, both as a primary condition and as a comorbidity.
This research report reviews the latest market trends and clinical updates impact AF management, as well as strategies identified from innovative programs to improve AF care delivery and program infrastructure.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
