Auto logout in seconds.
Continue LogoutOur research indicates that health plans are only the fourth most trusted source of health information, lagging behind physicians, pharmacies, and health-related websites. Surprising? Maybe not, but ironic none-the-less. Health plans have a wealth of insight and experience that could help members better navigate the health care system. The problem, however, is that health plans aren’t seen as a trustworthy source of health information by consumers.
Below, we review a case study in which New Mexico Health directly addresses this issue by leveraging community health workers (CHW) to influence member medication adherence in local communities. By doing so, they are engaging members through a trusted third party and positively impacting member health.
To read similar case studies and learn other strategies that our research indicates is critical to member engagement, download our complimentary resource Shattering the Member Engagement Myth Part Two: Health Plan Diplomacy.
Multiple strategies are at the disposal of plans to communicate to, and build relationships with, their members.
One strategy is to utilize community health workers. The American Public Health Association defines a CHW as, “a frontline public health worker who is a trusted member of and/or has an unusually close understanding of the community served. This trusting relationship enables the worker to serve as a liaison/link/intermediary between health/social services and the community to facilitate access to services and improve the quality and cultural competence of service delivery”.
By communicating with members through third parties, such as CHWs, plans can break down barriers, create relationships and start being seen as trusted sources for health information.
Case study: New Mexico Health Connection Partners with Community Workers
New Mexico Health Connection (NMHC), an 18,000 member co-op plan, is working with local partners to improve medication adherence. The plan pays Federally Qualified Health Centers (FQHCs) to hire community health workers who help NMHC members follow their care plan.
A CHW's close relationship with a member helps to bridge the trust gap that health plans have historically had with their members.
The CHWs help members remember to take their medication and can go into the member’s home to find any trouble spots that might arise. Working alongside the clinical staff, they can establish a relationship with the member and their family that helps to ensure care adherence.
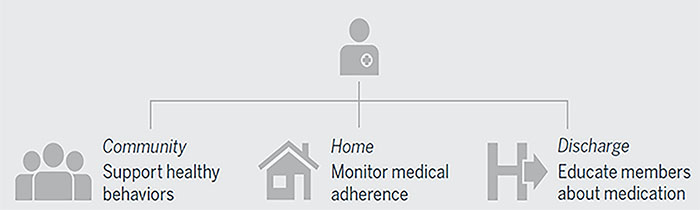
Though this won’t necessarily drive engagement to the plan, it can improve outcomes and experience—two things members are likely to remember when it comes time to renew.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.