Auto logout in seconds.
Continue LogoutThe challenge
In 1988, leaders at Family Care Specialists (FCS) Medical Group wanted to address the underrepresentation of Latinx (a gender-neutral term for people of Latino origin) people in health professions and leadership roles in East Los Angeles, California, while also addressing the local shortage of health professionals. At the time, Latinx people made up 80% of the local population but only 8% of physicians. The physician-to-patient ratio was 1:3,700, making the locality a federal Critical Health Professions Shortage Area.
The organization
FCS Medical Group has a high-quality safety net practice with four locations and over 120 staff, an independent physician association (FCS IPA) with a network of more than 340 physicians, and a family medicine residency program at Adventist Health White Memorial (AHWM) Medical Center, a safety net hospital. FCS serves 30,000 people in East Los Angeles. FCS operates health workforce programs to increase diversity, ensure placement of graduates in underserved areas, and develop future leaders.
The approach
In 1988, FCS established a family medicine residency program to recruit and retain graduates in medically underserved communities. FCS also partnered with local high schools, colleges, and community organizations to establish a health professions pipeline to support underrepresented minority students in pursuing clinical roles. FCS links students with academic enrichment programs, research opportunities, meaningful employment, and mentorship, among other supports.
The result
FCS has graduated 226 physicians from the AHWM family medicine residency program, 67% of whom resulted directly or indirectly from their pipeline program and 65% of whom identify as underrepresented minorities (URMs). And 30% of those graduates are in leadership positions. Health plans, medical groups, and health systems look to FCS as an exemplar in developing workforce programs to increase diversity in the medical professions and address physician shortages. FCS was the winner of Advisory Board’s 2021 Innovation Showcase: Strategies to Advance Diversity for their workforce development programs.
How FCS established a health professions pipeline so they could grow their own clinicians and leaders
In response to a critical physician shortage and a desire to increase Latinx representation in the clinical workforce, FCS established a family medicine residency and health professions pipeline to support students from high school to residency to medical practice and equip them with advocacy skills to serve as physician leaders after residency.
The five components
FCS health professions pipeline has been in the works for over 30 years. These five components constitute the keys to their approach since 1988.
In 1988, six board-certified Latinx family physicians co-founded Family Care Specialists (FCS) Medical Group to improve the quality of care available in East Los Angeles (East LA).
At the time, the community of East LA numbered 800,000 people. Eighty percent were Latinx, 50% spoke only Spanish, and 33% of adults were uninsured. The community was designated a federal Critical Health Professional Shortage Area (HPSA). A primary care (HPSA) is defined by the National Health Service Corps (a division of the U.S. government agency Health Resources and Services Administration) as having a population-to-provider ratio of at least 3,500 to 1. In 1988, the population-to-provider ratio in East LA was 3,700 to 1. Before FCS was founded, the region had only one board-certified family physician.
The FCS co-founders saw an opportunity to help address the shortage of board-certified family physicians, primary care nurse practitioners, and physician associates in underserved areas and simultaneously improve representation of racial/ethnic minorities in health care.
The co-founders of FCS grew up in East LA. Their own educational journeys exposed them to the value of peer support, advocacy, academic enrichment programs, and financial aid for disadvantaged students. This made them uniquely positioned to take on this mission.
In 1988, FCS established a family medicine residency program at Adventist Health White Memorial (AHWM), a safety net hospital, to train residents and primary care clinicians.
AHWM sponsors the residency and contracts FCS to run the program. FCS’ Family Health Center serves as the outpatient training site for the residency program. FCS physicians serve as program director and associate program directors for the residency program.
The AHWM Family Medicine Residency Program (FMRP) equips graduates to work in medically underserved areas, focusing on delivering culturally and linguistically competent services to vulnerable populations. The curriculum also includes leadership development, including learning through hospital committees, community partnerships, health policy work, and business situations.
The residency program’s charter class came from UC Davis School of Medicine, the alma mater of one of FCS’ founders. In following few years, the residents worked alongside the program directors to recruit classes of socially conscious young doctors from mostly California-based medical schools.
Alongside the residency program, FCS’ co-founders established the department of family medicine at AHWM. This served as the academic arm to support the residency program and helped recruit sub-specialists across the organization to teach the residents. FCS’ medical director serves as the chair of the family medicine department.
In 1996, FCS established its own Independent Practice Association (IPA) to contract with other primary care physicians—many of whom are graduates of the AHWM FMRP—and additional specialists to improve access to care for its patient population and recruit additional teachers in the surrounding community.
The residency program and department laid the foundation for FCS’ work to increase access to health professions for students from underrepresented racial/ethnic groups—and for those students to embark on a journey to return and serve their community as accomplished young professionals.
The residency program provided Family Care Specialists with one avenue to train more physicians. However, FCS leaders knew they needed to reach students earlier to increase the number of people considering health professions in the first place.
FCS cultivated a pipeline program with entry points in high school, college, medical school, and residency. This comprehensive pipeline program provides educational support to encourage students to consider careers in health care.
The pipeline is reinforced by MiMentor, a social media-based mentoring program focused on supporting aspiring health professionals from underrepresented minority (URM) groups. MiMentor was launched in 2014 by a group of residents, including two of FCS’ graduates. MiMentor now operates as an independent 501(c)(3) organization, but it is a common thread throughout FCS’ pipeline program and is the core source of mentorship support for those in FCS pipeline.
High school
FCS partners with three local high schools where most students are non-white and economically disadvantaged: Theodore Roosevelt Senior High School, Montebello Applied Technical Center (ATC) Magnet High School, and Francisco Bravo Medical Magnet High School. FCS physicians and residents provide health education, clinical shadow experiences, and career day support at these partner schools. When FCS representatives meet students who show interest in STEM or health professions, they direct them to MiMentor and connect them with the AHWM Charitable Foundation health careers program to link them to academic enrichment programs and scholarship information.
College
FCS partners with four local colleges—East Los Angeles College; California State University, Los Angeles; University of California, Los Angeles (UCLA); and University of Southern California (USC)—and multiple student organizations (including Chicanos/Latinos for Community Medicine) to nurture students’ interest in the health professions. Each year, FCS actively supports a cohort of roughly 40 college students from these schools who are enrolled in MiMentor, are on a pre-medical or other health professions track, and have roots in East LA. FCS helps coordinate paid research assistantships, summer jobs, and other academic programs. MiMentor offers these students mentorship, medical school application workshops, and career coaching. Once admitted to a health professional school, FCS’ program manager tracks the students’ academic progress and retention rates, and links them to scholarship programs, research assistantships, and clinical rotations at AHWM.
Medical school
FCS connects with the Latino Medical Student Association (LMSA), the Student National Medical Association (SNMA), and the Family Medicine Interest Groups at four local medical schools (USC, UCLA, Charles R. Drew University [CDU], and Western University of Health Sciences [WUHS] Pomona) to design useful academic enrichment, social, and organizing programs. At this point, students have already chosen to pursue a clinical career, so FCS’ focus is on supporting progress toward graduation and encouraging them to practice in underserved settings. FCS provides financial support for students to attend regional and statewide LMSA conferences and supports LMSA’s scholarship programs. Students may still work with FCS to coordinate summer research opportunities and work with faculty mentors on projects.
Residency
The entire pipeline serves as a feeder into FCS’ family medicine residency program. Of FCS’ 226 residency graduates to date, 67% directly or indirectly result from the organization’s partnerships with high schools, colleges, and medical schools. Because FCS intentionally partners with majority URM high schools and Latinx student groups, most of FCS’ residents are from underrepresented minority groups.
FCS relies on numerous partners to help underrepresented minority students navigate the many barriers on the way to becoming a clinician. FCS has cultivated an intentional partnership strategy and infrastructure to support students’ non-clinical needs.
FCS defines its core function as educating physician residents from underrepresented minority populations, and FCS identifies partners to serve other needed functions for students.
FCS maintains dozens of partnerships with community-based organizations, academic enrichment and tutoring groups, scholarship funds, afterschool programs, and more. This network of partners is informed by three decades of patient interaction and data analysis.
When FCS was founded, the leaders used the community-oriented primary care model to bring together patient information and public health data to understand community needs and existing community assets. FCS clinicians also use the HEADSS assessment to understand issues in adolescent patients’ lives. Together, these inputs inform a continuously growing database of FCS’ patients’ needs, such as housing, nutrition, mental health, and health education. Indeed, these are the social determinants of academic success.
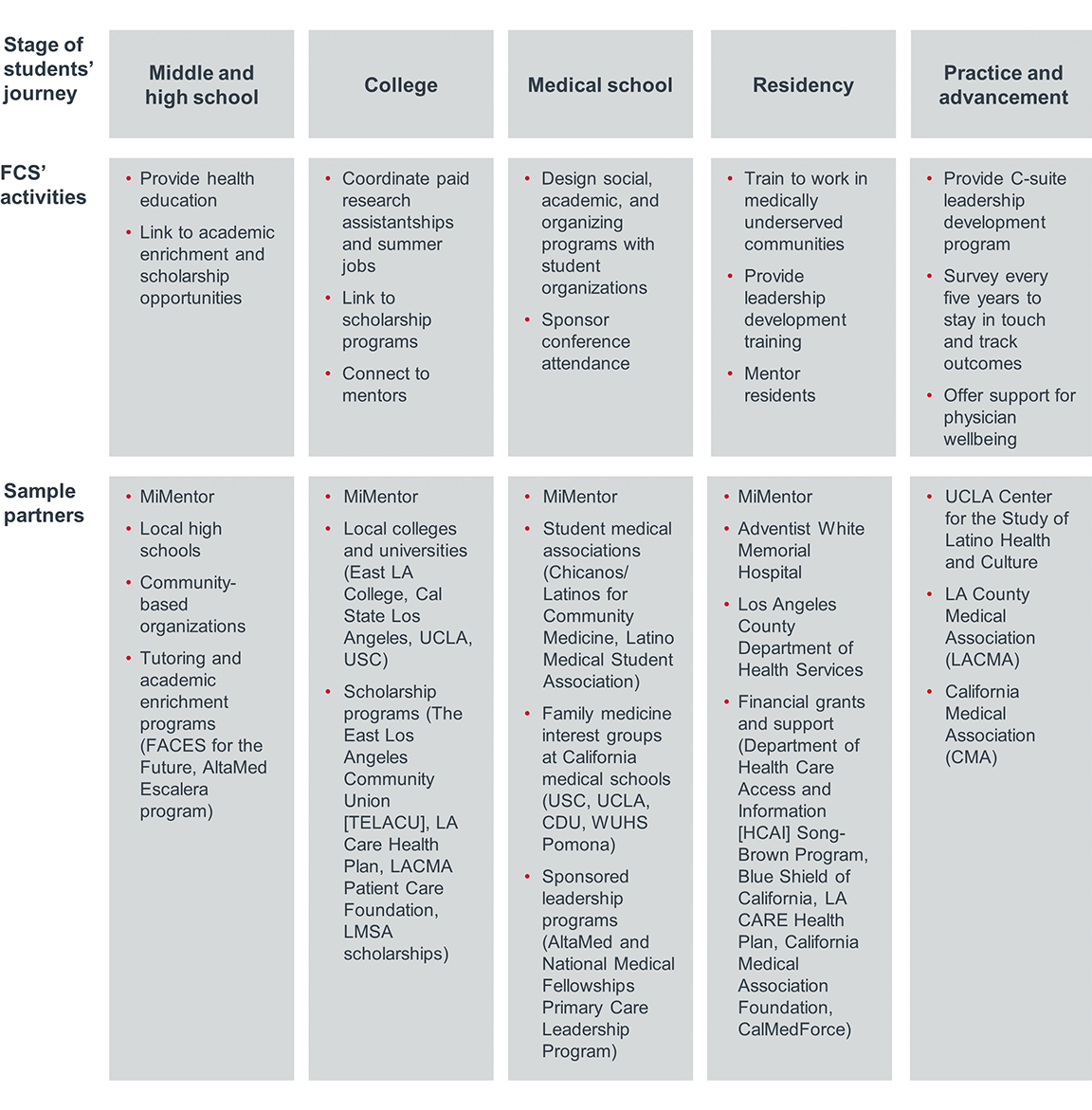
Outside of their core function of educating physician residents, FCS serves as a coordinator, linking patients and students to these partner organizations. Through grant funding, the AHWM Family Medicine Residency Program employs a program manager who maintains community partnerships and links students with partners for needed support. See the next page for an overview of how FCS engages and supports students across time.
The graphic below illustrates how FCS, in collaboration with numerous partners, supports students across their educational and career journeys. The activities and partners listed are examples but are not comprehensive. See the supporting artifact section for details on resources required to run FCS’ health professions pipeline activities.
Family Care Specialists’ comprehensive approach requires a way to stay in touch with students across their educational journeys, both to provide support when needed and to track outcomes to identify what is and isn’t working.
FCS tracks students through two primary mechanisms:
1. MiMentor
The MiMentor platform underpins the entire mentorship experience for FCS, providing continuity as students move through middle and high school to college and medical school.
While operating as an independent 501(c)(3) organization, MiMentor shares data with FCS to help the organization reach more students and track their progress. MiMentor has a database of approximately 10,000 students. This includes 2,500 URM medical students, with approximately 2,000 in California medical schools and 500 in other states.
MiMentor tracks the number of URM students originating in FCS’ service area, their high school graduation rates, success in college admissions (both community college and four-year institutions), retention rates, and success of professional school applications.
2. Follow-up surveys
Leaders at FCS and the program directors of the family medicine residency at AHWM survey residency program alumni three years after graduation and every five years thereafter to get recommendations on how to improve the residency curriculum, to track the long-term outcomes of the program, and to assess the practice support needed by graduates.
The health professions pipeline program receives funding from Family Care Specialists’ operational budget, but it also relies on financial support from several other sources. FCS’ leaders have sought to build relationships with diverse stakeholders with a vested interest in the organization’s success. When funding is an option, FCS builds a clear business case to secure investment. Detailed below are some, but not all, of the funding sources of the program.
Grants: FCS works with AHWM’s grant-writing team to secure grants to support two key positions for the residency program: the director of behavioral science, who oversees the high school health education programs, and the associate program director, who engages with college partners and family medicine interest groups. For example, in 2021-2022, FCS’ residency program received a $625,000 grant from California’s Department of Health Care Access and Information’s Song-Brown Program. The program provides funding to residency programs that admit underrepresented minorities and train and place graduates in medically underserved areas.
Corporations: In 2001, AHWM received a $1 million grant from Bank of America to formalize the pipeline program, in part because Bank of America recognized an opportunity to build connections with FCS’ residents and physicians and gain new banking clients.
Health plans: FCS has demonstrated success in training and placing physicians in medically underserved areas, which helps health plans better serve their members. FCS has received financial support for its pipeline and training from health plans including Aetna, Anthem Blue Cross, Blue Shield of California, Centene/Health Net, and LA CARE Health Plan. These major Medicaid health plans appreciate the positive impact the program has had on the health care safety net in Los Angeles.
How we know it’s working
To date, FCS has trained 226 graduates in the AHWM family medicine residency program with:
- 65% identifying as underrepresented minorities (URM)
- 67% directly or indirectly resulting from the FCS pipeline, including six former high school students
- 70% working in medically underserved areas
- 19% remaining in the local East LA community
- 30% holding leadership positions in health care
The 2021-2022 cohort of 24 resident physicians is 50% Latinx, 30% Asian/Pacific Islander, 8% African American, and 12% White, and their two chief residents are Latinx women. FCS Medical Group now numbers 29 primary care providers—62% are of Latinx descent and 45% are women.
Health plans and systems look to FCS as an exemplar in developing programs to increase diversity in the medical professions and address physician shortages. FCS won Advisory Board’s 2021 Innovation Showcase: Strategies to Advance Diversity for their efforts to advance representation in clinical and leadership roles in health care.
What’s next
In 2022, FCS plans to partner with the UCLA Center for the Study of Latino Health and Culture for a “Minority Physician Pathway to the C-Suite” project to expand the impact of their program with a focus on leadership development.
In January 2022, health care services and technology company Altais, a subsidiary of Blue Shield of California, finalized an agreement to acquire FCS. Altais aims to learn from FCS’ cost-effective, high-quality model of caring for low-income patients. Altais will provide capital support and a suite of technological tools, including those that will bridge the digital divide for their patients. FCS’ six founding physicians will continue to lead the group.
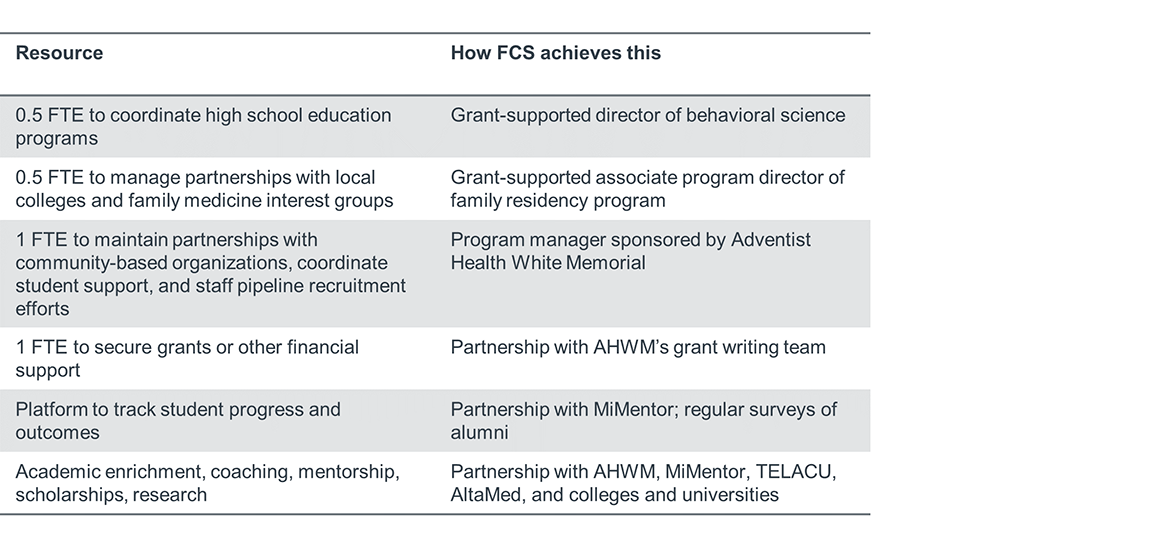
Resources required to support student programs
The table below offers an overview of the resources required to run FCS’ health professions pipeline activities. While not all of these resources are mandatory to start a similar model, these resources should be seen as goals for sustaining a similar approach.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
