Auto logout in seconds.
Continue LogoutOverview
Currently the diagnostic process for Alzheimer’s and other dementias is complex, costly, and capacity-constrained. This is mostly due to the fact that there is no single diagnostic test to confirm the disease. Additionally, there are structural barriers in place that inhibit access to testing: there is a lack of widespread billing and reimbursement for cognitive assessments, physicians have limited time to administer cognitive screenings, and there is an underlying reluctance to diagnose given the lack of a cure. Acknowledging that these are substantial barriers, we wanted to imagine a world where the health care industry overcame them.
How this would play out
Widespread screening of individuals would lead to earlier detection of the biomarkers for memory loss diseases, even before symptoms arise.
Why we believe this
There are numerous benefits that result from timely detection. First, it allows for earlier intervention, which could delay the progression of memory loss by controlling conditions that can accelerate its progression such as heart disease, diabetes, stroke, high blood pressure, and high cholesterol. It also allows for better medical, financial, and legal planning for patients and caregivers. Lastly, earlier detection would increase the number of potential clinical trial and early post-market participants (i.e., the first post-FDA approval users), leading to increased innovation around treatments or cures. Post-market participants play a particularly important role in generating real world evidence since they are the first to use the drug after it has made it through clinical trials.
Related resource
Blog: Why a breakthrough cure for memory care disorders likely isn't coming soon
How this would play out
Primary care practices would likely have to bear the burden of screening volumes, due to the relative lack of dedicated dementia care specialists like geriatricians, neurologists, and geriatric psychiatrists.
Why we believe this
Many experts argue that primary care practices should handle routine cognitive screenings as part of the annual wellness visit. However, for primary care practices to meet the demand for universal early screening they would need a combination of less laborious screening technologies and more creative deployments of their own care teams. Nurse practitioners and non-clinical staff, like front desk administrators, can be trained to administer behavioral questions, test for cognitive skills, and provide education and support following the patient’s appointment. This streamlines the screening process and helps everyone to work at top of license.
Related resource
Case study: How Carilion Clinic used workforce and coding techniques to overcome cost challenges in memory care
How this would play out
Patients and caregivers will need access to educational resources and care management support following diagnosis.
Why we believe this
Community-based organizations, Medicare programs like PACE (Program of All-Inclusive Care for the Elderly), and MA supplemental benefit packages often provide this kind of support for individuals with dementia and their caregivers. These organizations will be pressured to assess their budgets to meet the increased need in resources for those with memory loss if better, widespread screenings were implemented.
How this would play out
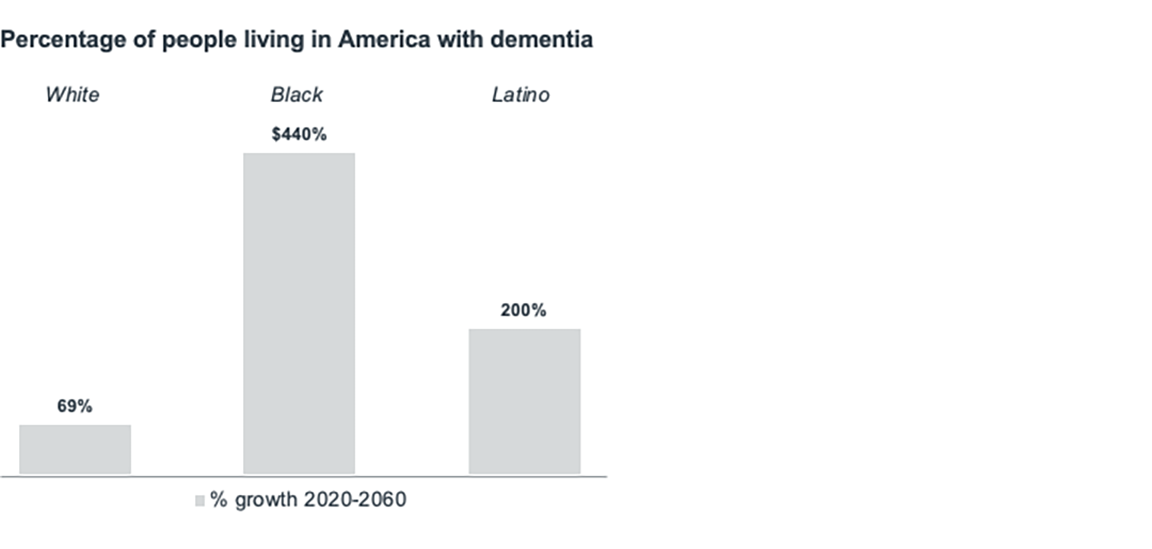
The prevalence of dementia disproportionately impacts women as well as communities of color. Better, widespread screening would enable providers, drug manufacturers, and community-based organizations to improve their outreach to diverse populations to raise awareness on the benefits of early detection.
Why we believe this
Lower rates of early diagnosis in under-represented groups is not due of lack of interest, but rather results from a need to overcome a lack of access to information. A more diverse pool of individuals could also mitigate equity issues downstream in the clinical trial space. Historically, clinical trial populations for memory care therapies have been disproportionately wealthy and white; however, diagnosing more diverse populations could lead to more diverse research participants and the collection of better data on treatments.
How this would play out
Employers and commercial payers will have to consider the implications of more pre-Medicare beneficiaries being diagnosed with memory care diseases.
Why we believe this
Individuals who continue to work as their disease becomes symptomatic may need additional benefits, including paid sick leave, short-term disability benefits, and a flexible spending account. Medicare Advantage plans would have a better sense of how many of their beneficiaries are diagnosed, even before symptoms may be triggered. This would enable them to cover therapies and practices that would save them money as their members’ diseases progresses. Payers will have to think through how to create or structure strategic partnerships to maintain effective costs for memory care treatments—especially since providers may need help preparing for the influx of diagnosed individuals. Many plans are already working with home care providers to better manage patient populations, so this could be a good avenue to carve in at-home supports for memory loss.
Although the implementation of accurate, cost-effective, and widespread screening would be a net positive for patients, it would challenge some parts of the industry. While this might seem like an impossible future, the world is moving fast in this direction. There have been rapid developments in using blood tests to measure the proteins indicative of Alzheimer’s symptoms. Also, we also know that the rapid aging of the population and increased dementia is going to push more research to this space. Stakeholders will have to prepare and react to this changing environment.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.

