Auto logout in seconds.
Continue LogoutRecently, Advisory Board convened a group of cross-industry leaders—representing providers, health plans, pharmaceutical companies, and other suppliers—to talk about the market forces that will shape the future of cancer care. We've synthesized the key takeaways from our in-depth discussions of precision medicine and value-based care below.
Infographic: Envisioning the future of cancer care
The workshop in brief
After brief introductions, workshop attendees were presented with two scenarios across the day—precision medicine and value-based care. For each scenario, individuals placed a mark on the spectrum indicating where they thought we stand today, where we'd be in an ideal world, and where we will be by 2025.
As a group, we then discussed barriers, opportunities, and the impact on patient care.
1. Precision medicine
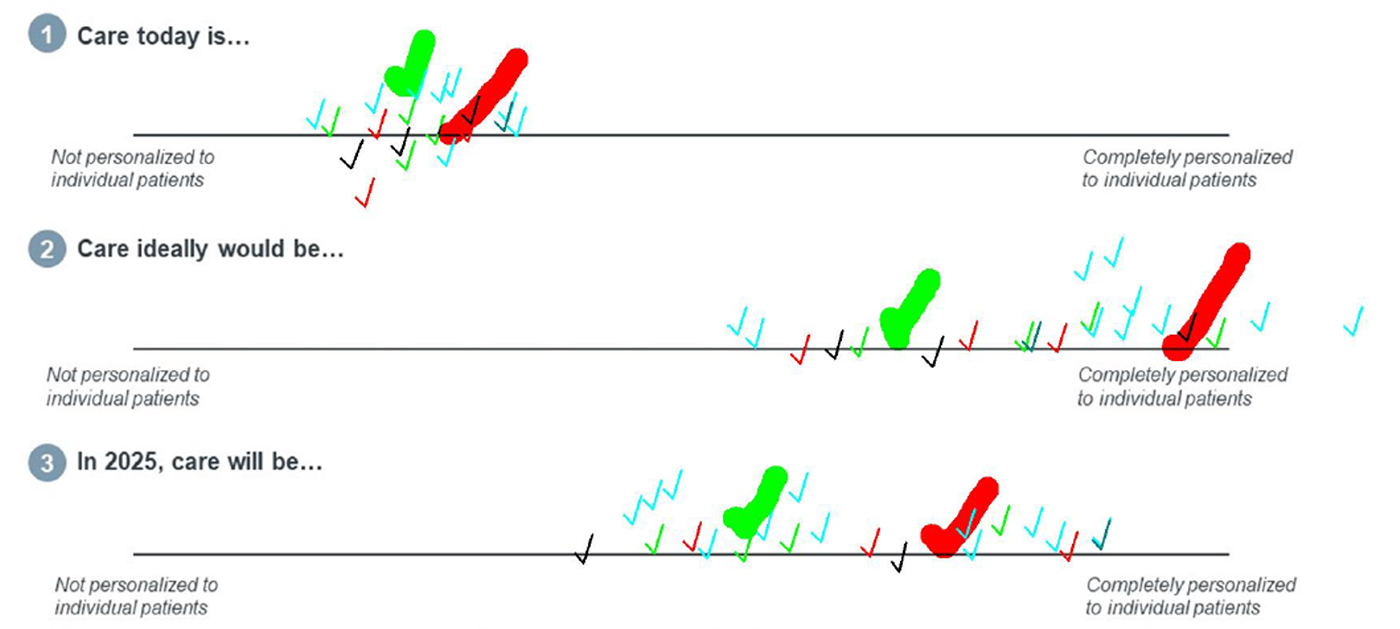
Arguably, among all the factors impacting oncology, the rapid evolution of precision medicine will have the biggest impact on how we deliver and pay for cancer care. Attendees agreed that we are early on this journey with significant opportunity in the next five years to deliver care that is more personalized to the individual. Three key themes emerged during the conversation:
Our scientific understanding of precision medicine is evolving faster than reimbursement mechanisms to pay for it. Despite widespread excitement for precision medicine advances across all stakeholders, there are clear risks to providers in offering therapies that plans are wary of covering at all or at full cost. Take for example CAR-T cell therapy. From the drug manufacturers' standpoint, more organizations should be offering this to their patients. However, given the resources and expertise needed, in addition to limited reimbursement, providers pushed back that they are set to lose money on CAR-T patients who aren't enrolled in a clinical trial. On their end, plans are still understanding the threshold of evidence needed to support robust coverage decisions for these new and high-cost therapies.
Providers need support implementing precision medicine appropriately into patient care. With the explosion of diagnostic tests and treatment options, precision medicine is likely to add steps to the patient pathway, potentially delaying care, confusing patients, and overwhelming providers. According to cognitive scientists, the human brain has the capacity to incorporate about five facts into the decision-making process. Due to new technologies, such as biomarker testing and genetic sequencing, the number of facts relevant to clinical decision-making in oncology are growing exponentially. In response, stakeholders across the industry need to work together to create integrated, point-of-care decision support solutions that help all providers—from the most research-focused to community-based—select the right tests and treatments for their patients.
The field needs to ensure all patients who stand to benefit from precision medicine are able to receive it. As with most innovations, how to ensure equitable access was voiced as a common concern. First is the question of which communities and patients have access to the organizations providing cutting-edge therapy. Most trials and robust precision medicine programs are housed within academic medical centers, making it paramount to have systems in place where rural and/or smaller non-academic programs can identify and refer patients if they are not able to offer specific therapies or trials.
2. Value-based care
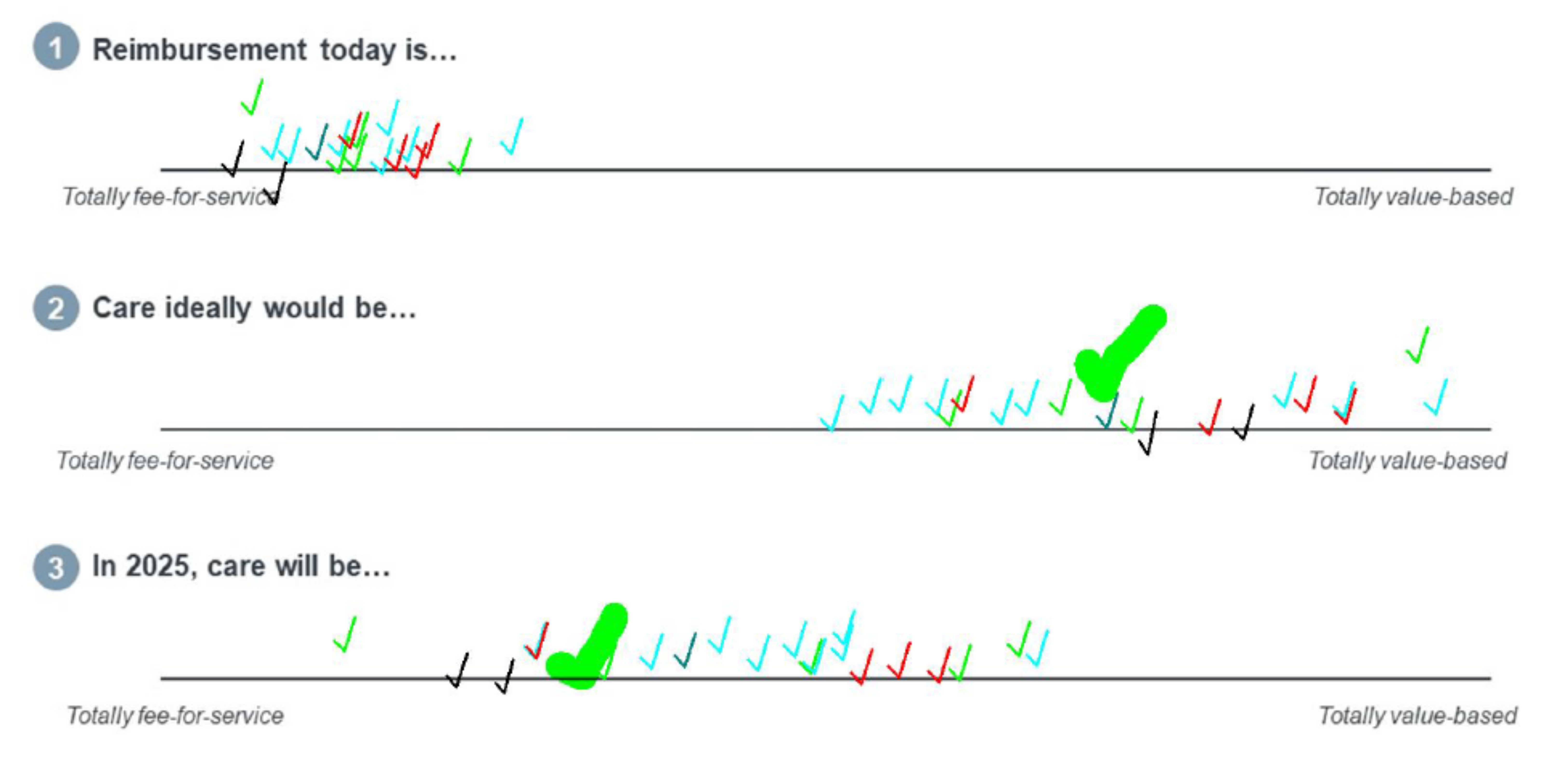
Given the rising costs of cancer care and the aging population, we've seen heightened interest in exploring value-based care models from both private and public payers—to varying degrees of success. Our workshop attendees generally agreed that oncology still operates largely in a fee-for-service world, with widely diverse opinions on how much care should and will be value-based even five years from now.
The three main areas of discussion included:
Stakeholders don't have a shared definition of "value" in cancer care. At the most basic level, stakeholders across the industry have ill-defined and inconsistent definitions of what "value-based care" in oncology means. This lack of a shared definition and vision hinders progress and has resulted in disparate pilots and tools being used in isolation. Furthermore, as treatment improves, cancer is now a chronic disease for many, underscoring the importance of tracking and reporting long-term outcomes and refocusing the timeframe by which we measure "value."
Providers call for upfront financial investments to support care transformation. Given that providers aren't currently reimbursed for many of the elements deemed necessary to drive value, such as nurse-led symptom management and navigation, many attendees called out the importance of plans and providers working together to fund care transformation initiatives. Cancer-specific payment models can also be extremely risky for providers as a small number of outliers can drastically drive costs. What's more, due to the diversity of cancer diagnoses, value-based programs often ask stakeholders to commit significant resources to a program that only affect a small number of patients. Many participants noted that no one stakeholder seemed to be willing to front the costs for transitioning from a fee-for-service to a value-based care world. Although the financial and quality benefits of operational goals like reducing unnecessary care sound appealing, many providers are concerned about their financial interests in a value-based world and many plans have invested resources in these efforts without seeing significant savings.
Each stakeholder group needs to commit to cultural change and honest communication to move the dial on value-based care. From the plan perspective, it is incredibly difficult to bring all the necessary players together and, despite having invested in value-based contracting teams, very few programs ever materialize. From the provider perspective, organizational and clinician commitment remains challenging, made even more difficult by the current burnout and change fatigue most health care organizations are facing in the wake of Covid-19. Interestingly, pharmaceutical companies were very transparent about their interest but shortcomings in participating in value-based arrangements, whereby they also take on financial risk based on a drug's outcomes in the real world compared to its performance in clinical trials. Coming to agreement with all necessary parties, having executive buy in, picking the right drugs and outcomes to measure, and then collecting and analyzing the data are just a few of the very real hurdles making it difficult for pharma to share financial risk for expensive new therapies.
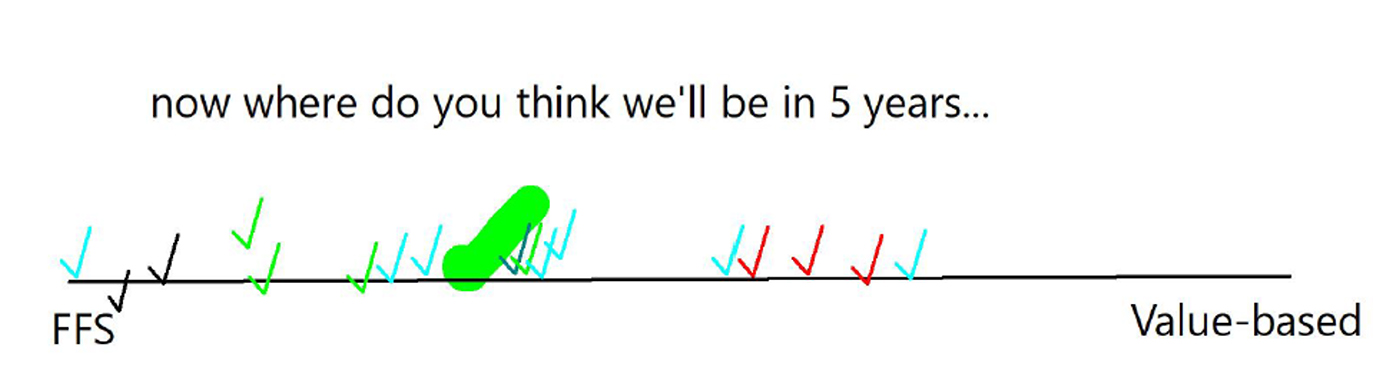
Given the very complex and deep-seated issues surfaced in our conversation, the group then walked back their original estimates of how much progress we'd make in the next five years.
Mallory Kirby contributed to this post.
About Advisory Board
For more than 40 years, we've helped executives and future leaders in health care work smarter and faster by providing provocative insights, actionable strategies, and practical tools to support execution.
With 40+ years of experience, a team of 250+ experts, and a network of 4,900+ member organizations that span the payer, provider, and supplier industries, we support life sciences firms’ commercial and medical leaders with research and educational resources that develop market strategy, enrich customer insight, and more.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
