Auto logout in seconds.
Continue LogoutBy: Natalie Trebes and Sally Kim
Capitated payment models put the responsibility for cost management on providers’ shoulders. That can mean more efficient use of care—but these models also run the risk of discouraging preventive care.
HealthNow New York, a Blues plan in upstate New York, recently launched a hybrid payment model called BestPractice to get the best of both worlds: assured access to preventive care and efficient management of ongoing conditions. We spoke with HealthNow’s Chief Network Officer and SVP Ron Mornelli and Medical Director and VP Dr. Kirk Panneton to learn more.
Q: At a high level, what does the new BestPractice reimbursement model look like?
Mornelli: It’s a hybrid reimbursement model we’ve launched for primary care providers (PCPs), that combines fee-for-service (FFS) and capitation payment structures. We’re reimbursing certain preventive services like annual physicals and immunizations on a FFS basis. But we’re capitating services related to condition management under a monthly, risk-adjusted rate.
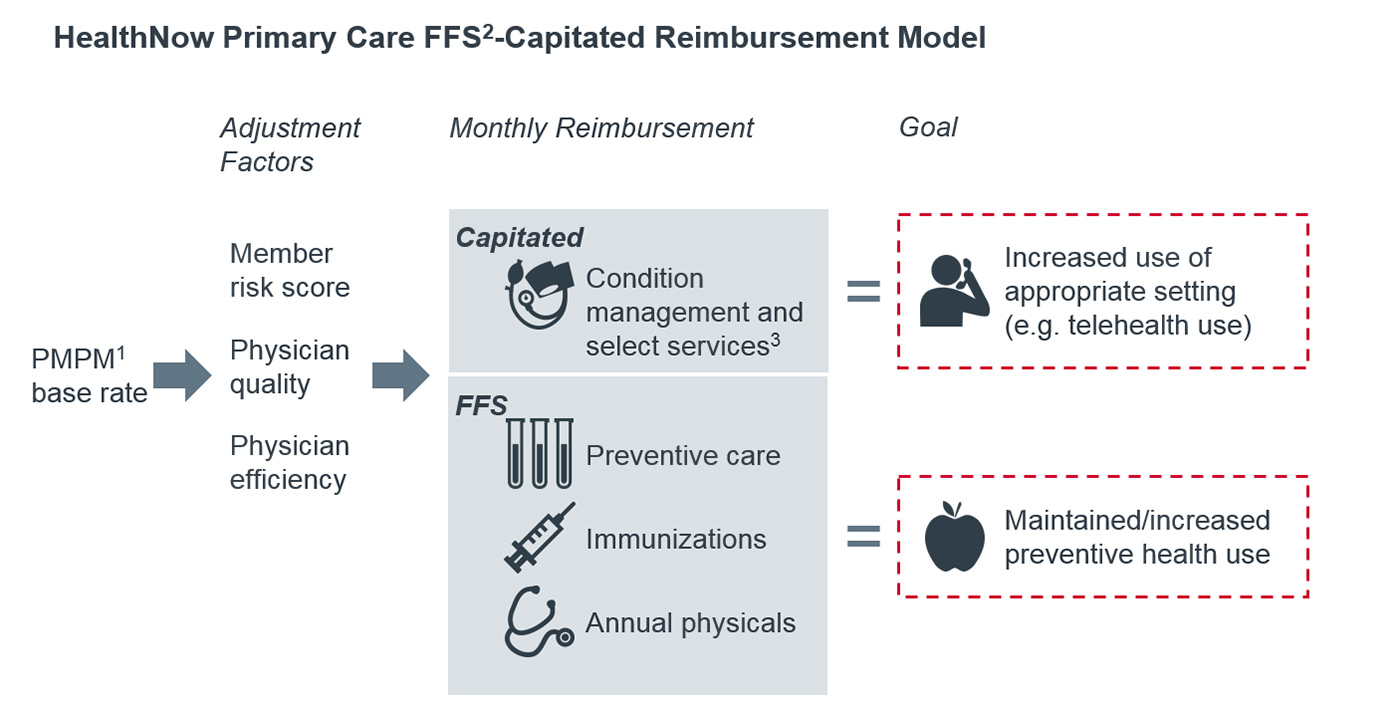
1) Per member per month.
2) Fee for service.
3) Capitated codes include the following code types: allergy testing/immunotherapy, evaluation and management, EKG, hearing and speech exams, lab, non-classified, ophthalmology, pulmonology and radiology-non MRI.
Q: Highlighting FFS reimbursement in a value-based payment model is a little different than what we typically hear about. Why is that important, and how did you decide what to cover under FFS and what to cover with capitation?
Mornelli: Fee-for-service is fee-for-value when it’s reimbursing care you want to encourage—the preventive services, in this case. We use professional societies to define preventive services but in general, any PCP service that isn’t capitated will be reimbursed on a FFS basis. High-end services that can be done outside the office in urgent care centers—like simple lacerations and treating bee stings—are also reimbursed through FFS, because we want to incent that care in the more cost-effective primary care setting. Certain evaluation and management (E&M) services and select labs and tests are reimbursed through risk-adjusted capitation.
Q: So why now—what made you decide to launch this new reimbursement model?
Mornelli: The doctor-patient relationship is essential in delivering care, but traditional payment models don’t always recognize its value. As we transition to population management models, we want to put this relationship at the center and give PCPs discretion over how they provide services to their patients. With this model, we wanted to make sure that incentives were aligned to enable PCPs to manage entire care plans. For example, one of our specific goals was to give doctors a way to manage member issues over the phone. So we made sure the PMPM rate would cover care via phone or other telehealth media if necessary.
Q: Changing reimbursement isn’t always an easy sell. How did you get providers on board with the new model?
Mornelli: We went to great lengths to hold community meetings and send representatives to PCP offices to provide training and education on the model. We held 10-15 meetings open to physicians and staff months before the model went live. In addition, representatives trained in the model went out over that same period to meet with each office to make sure that they understood the incentives and goals of the model. In the end, this significant undertaking made the transition easier.
Q: How will you define success for this program?
Panneton: We don’t expect total cost of care to change that much, but we expect the costs to shift. We’d rather spend more on PCP visits than on unnecessary ED visits, hospitalizations, or other types of utilization.
Mornelli: Also, with more telehealth visits, there’s more capacity for PCPs to fit patients in their office. When patients are managed at the most appropriate setting, wait times for care will decrease across the board. As PCPs are reimbursed for providing the right service, we expect member access to increase. Telehealth is just one way different free structures can impact access.
Q: Now that you’ve made the initial transformation, what’s the next step for BestPractice?
Panneton: Currently, reimbursement in BestPractice is adjusted for provider quality compared to the peer group, as determined by HEDIS compliance. In 2018, we’re going to add an adjustment for relative efficiency, or how well providers use available resources to manage the total cost of the patient panel including both direct and indirect care. We will make sure to be transparent about this measure because providers already ask us “why is another provider in my practice considered more efficient than I am”?
More from the Advisory Board
Visit Advisory.com/healthplans to see what we’re researching.
Join over 4,000 health care organizations and become an Advisory Board member today: Learn how.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
