Auto logout in seconds.
Continue LogoutThe challenge
For patients diagnosed with breast cancer, up to 30% develop stage IV or metastatic breast cancer (MBC), which often requires unique treatment and symptom management. MBC patients may not always receive the tailored care needed to manage their medical and psychosocial needs, including geriatric patients or those who experience sociodemographic disparities. Without deliberate coordination and interdisciplinary care, patients may experience poor health outcomes.
The organization
University of Pittsburgh Medical Center (UPMC) is a healthcare provider and insurer that operates 40 hospitals and over 700 physician offices and outpatient centers. Headquartered in Pittsburgh, PA, UPMC is well-known for its transplant, cancer, neurosurgery, psychiatry, rehabilitation, geriatrics, and women’s health centers.
The approach
To support its MBC patients, including geriatric patients, UPMC created a nurse-driven quality improvement and primary palliative care intervention program in 2016. The Support/Education/Advocacy (SEA) Program of Care for Women with MBC connects patients with existing support and educational resources through a standardized assessment process. Meeting in a weekly huddle, a dedicated interdisciplinary clinical staff conducts patient chart audits to track care needs, connect patients with resources, and ensure patients receive the recommended resources.
The result
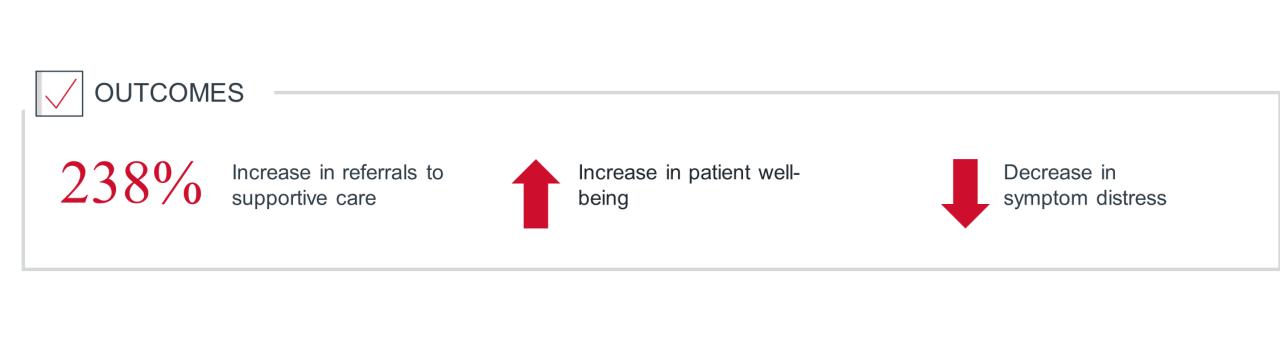
The SEA program has led to improvements in MBC patient-reported outcomes, fewer calls to the clinic, and fewer visits to the emergency department according to UPMC leadership. Doctors also found success in better identifying patients who may benefit from supportive care referrals, like social work and palliative care, while also being cognizant of time and workload constraints of clinical staff. UPMC has found this particularly valuable for vulnerable patients and it’s gone a long way in improving care for senior patients with MBC treated at their center.
How UPMC developed the metastatic patient huddle
Dr. Margaret Rosenzweig, a professor at the University of Pittsburgh’s School of Nursing, oversees a team of researchers who developed and maintain a database of 2,000 MBC patients in collaboration with UPMC Magee-Womens Hospital. Funded by various sources, this database became an instrumental resource for quality improvement projects and doctor inquiries.
After using the database to retrieve patient information over time, Dr. Rosenzweig noticed frequent reported symptoms of financial and physical distress among patients with metastatic breast cancer. This was true for all patients with metastatic breast cancer and can be particularly concerning for seniors who are more likely to suffer from other health conditions on top of their cancer diagnosis.
She considered available clinical resources to assess what patients needed and determined how those needs could be met. To coordinate interdisciplinary care in response to fluctuating patient needs, she conceptualized the weekly metastatic huddle — a nurse-driven, quality improvement, primary palliative care intervention program. This huddle supported all patients with metastatic breast cancer and was particularly supportive for vulnerable patients such as seniors.
The three steps
To operationalize the weekly metastatic huddle UPMC leadership established three steps:
Establishing the metastatic huddle began with defining its structure: the flow of weekly meetings and the sources of funding. UPMC first developed the preparation and execution process of the weekly meeting.
Once this was finalized, UPMC secured a local grant funded by Susan G. Komen for the Cure that covered staffing and operations costs. One part-time nurse was hired to review the charts for the weekly meeting, lead the meeting, and send reminders of follow-up referrals and support.
To obtain sustainable future funding and avoid long-term financial constraints, leaders sought out a project champion — someone who saw the potential impacts of the program. The project champion collaborated with leadership and the nursing staff to devise the concept of funding the program through a clinical career ladder.
Philanthropy is a great source of short-term funding to get started. There are usually many breast cancer philanthropy groups locally that can provide support.
The UPMC project team needed to determine who would be most useful to have at these huddles. Supportive care staff like palliative care and financial services attend because the clinical nursing staff benefits from discussing the supportive care needs of their patients in a collaborative setting.
According to Dr. Rosenzweig, palliative care and financial services can help identify which patients may benefit from their services, or discuss what support they have provided to patients so far. It is also an opportunity to discuss care options directly with the nursing staff and better understand what support is best for all patients, including vulnerable populations like geriatric patients.
The huddle also plans to include more clinical trial staff in the future. This could raise awareness for all care team members on the latest clinical trials treatment options. This increase in awareness may result in better treatment decisions for patients discussed within the huddle.
The SEA program’s weekly huddle include interdisciplinary attendees
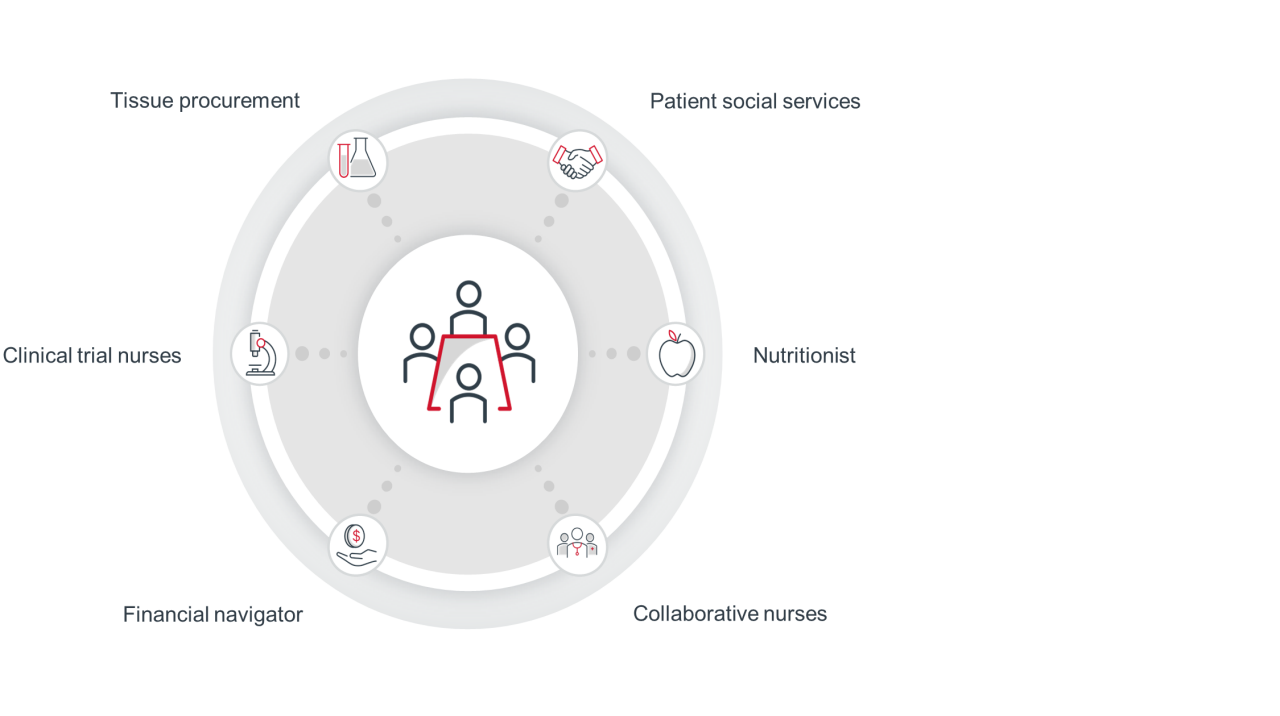
To make the weekly huddle productive, UPMC had to align the program’s goals among the stakeholders and determine a meeting time that worked for everyone. This included clinical nurses, palliative nurses, collaborative nurses, and social services, among many others.
Each stakeholder has a unique set of daily priorities. The project champion assumed the earlier the meeting, the more convenient it would be for participants. However, personal responsibilities prior to starting the work-day meant early mornings weren’t best for everyone. To address this, the project champion first worked to find a meeting time that worked for best for all stakeholders.
Next, the project champion centered stakeholders on the potential impact this huddle could have on patient outcomes. This helped ensure staff and leaders remained supportive and consistently joined and participated in huddles. The huddle is intended to support all patients, particularly vulnerable patients such as seniors. Centering on support for vulnerable patients helped keep UPMC stakeholders aligned on a common goal and engaged in the huddle.
Utilizing talent and agency
Getting ready for and executing the weekly huddle required the effort of multiple people. With support from Dr. Brufsky, Co-director of the Comprehensive Breast Cancer Center at UPMC, Dr. Rosenzweig sourced preparation assistance from multiple stakeholders.
They were trained to review MBC patient charts prior to meetings, which removes much of the heavy load from the program champion or the coordinating nurse leading the huddle.
Another option UPMC considered for funding support was making the program worth 10% of a nurse’s salary. In other words, preparing for and running the meeting would comprise a portion of nurse’s duties on a given day/week.
UPMC’s four-step process for the weekly huddles
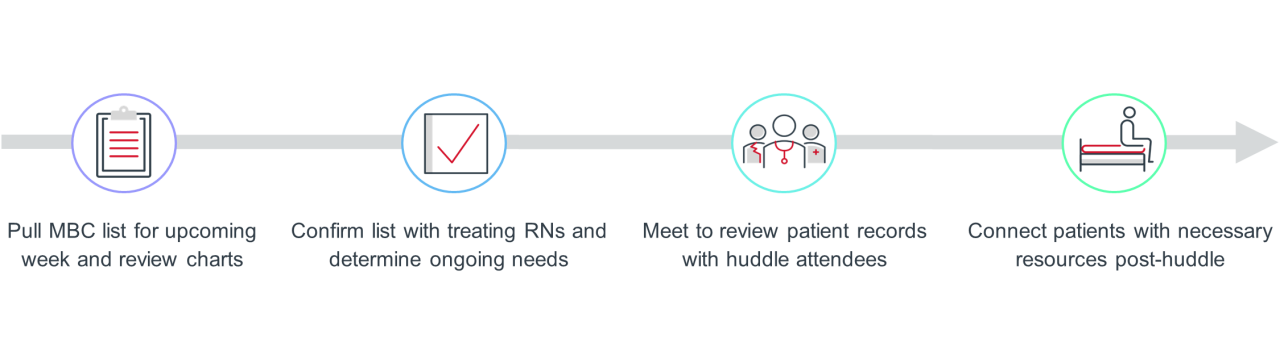
Generate MBC list for the following week and review charts
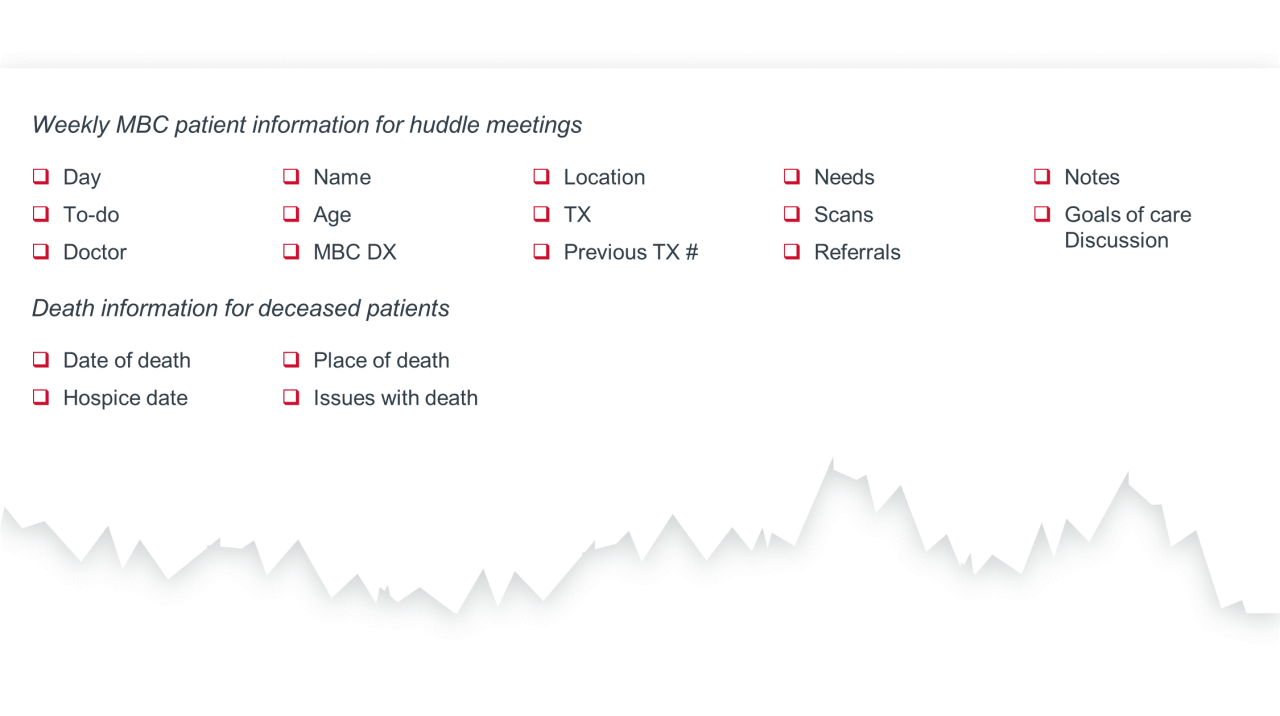
The week before a meeting, a data manager combs through the database of MBC patients and compiles a list of those scheduled to come into the clinic, those currently in the hospital, and those who have passed away.
Then, this list is sent to the lead nurse and preparation assistant. Collectively, they review every patient record and update a corresponding Excel spreadsheet for the meeting.
Confirm list with treating RNs and determine ongoing issues/needs
The MBC patient list is shared with the clinical nurses who work with the doctors overseeing these patients. They review it in detail and write up any concerns they have or opportunities to discuss referrals to social service, palliative care, financial navigation assistance, or other supportive services.
UPMC sees value in this step because nurses come prepared to the weekly huddles with the most pressing care needs to review, which streamlines the process of connecting patients with effective support.
Meet to review patient records with clinical staff and stakeholders
During the meeting, the lead nurse starts from the top of the list and shares each patient’s most up-to-date information. This includes age, symptoms, scans, treatment, and pressing needs. Different departments chime in based on this information with their latest updates, from social services and financial navigation to nutrition and tissue procurement.
At the meeting’s closure, they review any recent patient deaths and assess the quality of their end-of-life care. Leaders found discussing end-of-life treatment decisions and supportive care in an interdisciplinary setting helps the team move forward on the same page and support more standardized decisions during end-of-life care.
The huddle serves many patients by ensuring continued supportive care needs are met and adapted if needed. UPMC leaders believe the huddle is especially helpful for patients with chronic issues that change overtime, or for patients who present new, complex care needs.
EXAMPLE: UPMC’s interdisciplinary huddle supports the needs of seniors with MBC
A geriatric patient seen in the clinic said she was taking her medications accurately, but she couldn’t relay her medication schedule when asked. She also reported higher levels of distress at her monthly visits with her doctor.
The woman’s primary caregiver was her daughter, though she didn’t accompany her mother to her clinic visits because they didn’t live in the same city. This patient’s needs and concerns were discussed in the weekly huddle, which resulted in a meeting with the woman’s primary caregiver and social services.
At this meeting, the patient admitted to not taking her medication because she was struggling to remember and care for herself independently, while her daughter emphasized the stress of caregiving from another city.
Through interdisciplinary discussion, they collaborated with a non-profit elderly support agency to offer personal care through cooking, cleaning, and medication management. UPMC helped ensure this geriatric patient took her medications accurately, decreased self-reported distress, and decreased the stress of the caregiver.
Connect patients with necessary supportive care or resources post-huddle
At the end of the huddle, the lead nurse compiles notes from each patient discussed and includes necessary follow-up. This information is shared with the huddle attendees, and supportive care team members connect with patients as needed.
For example, if a patient was identified as needing to connect with financial navigation to discuss financial planning for care, a financial navigator will connect with that patient and address those needs.
Since the huddles occur weekly, each department will follow-up on how supportive consults went and if there are ongoing needs they are working to resolve. For example, the financial navigator will update the huddle on the consultation with patient needing financial planning support and how they will continue to support that patient.
In a way, the weekly huddles function as a forcing mechanism — huddle attendees know they will have to provide an update on the support they’ve provided to patients if flagged in the previous huddle. This motivates them to quickly connect with the patient and create a supportive plan to discuss during the following huddle.
Patient status and concerns documented prior and during weekly huddle
How we know it’s working
Over time, UPMC’s patient care teams have identified a variety of measures help evaluate the success of the huddle, including:
- Pre-patient reported outcome of MBC cohort and individual patients
- Post-patient reported outcome of MBC cohort and individual patients
- Referrals
- Quality assurance
UPMC leaders report that the weekly metastatic huddle has become a tool in improving referrals to social services, palliative care, and potentially improving subsequent patient-reported outcomes.
After initiating the program, they reported fewer calls to the clinic and visits to the emergency department. The team continues to meet weekly and on average generates five patient referrals a week to either palliative care, social services, nutritional counseling, or financial navigation.
Physicians treating patients with MBC1 also found success in better identifying patients who may benefit from supportive care referrals, like social work and palliative care, while also being cognizant of time and workload constraints of the clinical nursing staff. Patients discussed in the huddle also experienced increased well-being and decreases in symptom distress.
Connect patients with necessary supportive care or resources post-huddle
In addition, this program has served as a strong impetus for future work. UPMC recognized that despite the weekly huddles, Black MBC patients in poor communities were still struggling.
As a result, UPMC began training community center doulas to walk with patients through their MBC care both in and outside of the clinic setting. This effort was first funded internally, and now a larger pilot study is being funded by a philanthropic organization.
Going forward, UPMC plans to incorporate changes to the metastatic weekly huddle program:
- Concentrating on the assessment at the time of a patient’s MBC diagnosis to proactively utilize supportive services.
- Improving early-stage assessment.
- Tracking the number of clinical trials accrued if clinical trial staff become a consistent member joining huddles.
The weekly interdisciplinary meeting focusing on supporting patients with metastatic breast cancer in our practice is truly patient-centered care. The meeting ensures that each patient, over their disease trajectory, is assessed frequently and proactively for supportive care needs.
The interdisciplinary huddle supports an organization’s most vulnerable patients by better identifying supportive services that could improve care. Given cancer incidence rises steadily with age and the U.S. population is aging rapidly, geriatric patients are a top concern in oncology. Today’s seniors can be particularly vulnerable as they may face challenges like financial distress, increased comorbidities, insufficient caregiver supply and skillsets, and systemic care inequities. Strategies like this can support seniors’ challenges in a variety of ways. The inclusion of social workers and financial navigators can help identify seniors struggling with financial distress and implement solutions to support.
The interdisciplinary structure allows collaboration on opportunities to better support seniors with comorbidities. Organizations may consider standardizing discussions about seniors’ caregiver status and use social workers and nurses to better support caregivers experiencing distress. To address care inequities, programs could educate huddle members on the potential impacts of ageism on cancer care, and on understanding social determinants of health and their root causes. This will become more important as the senior population continues to diversify.
Additional considerations in geriatric oncology care
- Geriatric risk assessment: The geriatric risk assessment can help detect aging-related health issues missed in routine oncological work-ups such as fall risk or cognitive deficit.
- Empower and support caregivers: 75% of caregivers for seniors' report experiencing caregiver burden. Proper education on how to manage a patient’s medication side effects and symptoms can help alleviate caregiver distress.
- Health equity strategy: Ageism can potentially negatively impact oncology care through cancer screening bias and undertreatment. Additionally, the senior population is diversifying with a projected 115% rise in racial or ethnic minority seniors from 2019-2040.
Emily Schmidt wrote this report. Liam Frieswick and Binqi Chen contributed to the research.
This report is sponsored by Pfizer, an Advisory Board member organization. Representatives of Pfizer helped select the topics and issues addressed. Advisory Board experts wrote the report, maintained final editorial approval, and conducted the underlying research independently and objectively. Advisory Board does not endorse any company, organization, product or brand mentioned herein.

This report is sponsored by Pfizer. Advisory Board experts wrote the report, maintained final editorial approval, and conducted the underlying research independently and objectively.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.