Auto logout in seconds.
Continue LogoutHospitals and health systems often struggle to address all of a polychronic patient’s clinical and non-clinical needs during a hospital stay, which can negatively impact both clinical quality and patient experience.
Download this brief to learn how to elevate support for polychronic patients and simultaneously improve quality and experience during—and after—a hospital stay.
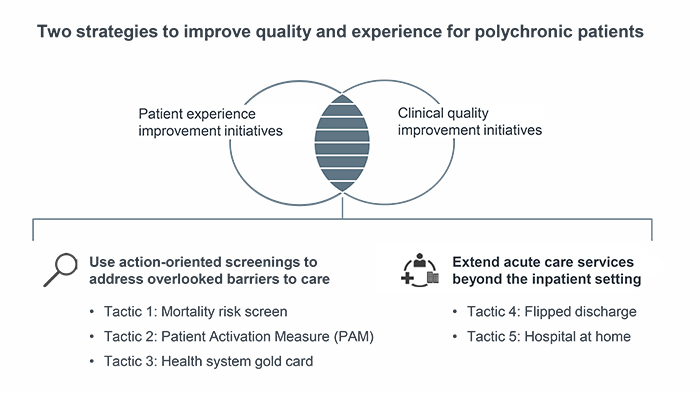
To deliver a quality-driven experience for polychronic patients, physicians must proactively identify chronically ill patients and their needs—and match them to tailored interventions. Through our research, we identified two strategies that hospitals and health systems can use to uncover and better address polychronic patients’ needs in the inpatient setting.
Five tactics to improve quality and patient experience for polychronic patients
Executive Summary (p. 4):Redefining the patient experience ambition
Strategy 1: Use action-oriented screenings to address overlooked barriers to care
Proactively screen polychronic patients for commonly overlooked clinical and non-clinical risk factors and consistently link patients to tailored support during and after the inpatient stay.
- Mortality risk screen (p. 8): Identify patients who are at risk of 30-day mortality at the decision to admit and match them to a standardized set of clinical interventions.
Related resources:
Published studies on the mortality risk screen
St. Joseph Mercy's mortality risk screen care bundles and interventions
Additional evidence to quantify the value of a mortality risk screen
- Patient Activation Measure (PAM) (p. 13): Measure patient activation—a patient’s underlying knowledge, skills, and confidence to manage their health—to inform their care plan.
Related resources:
Insignia’s Patient Activation Measure questionnaire
Additional evidence to quantify the value of the PAM
- Health system gold card (p. 17): Develop a comprehensive, cross-continuum program to support patients with a specific chronic condition and high inpatient utilization.
Strategy 2: Extend acute care services beyond the inpatient setting
Shift acute care services to patients’ homes to help reduce readmission rates and improve experience.
- Flipped Discharge (p. 22): Move elements of the discharge process from the hospital to the home setting to decrease length of stay and improve patient satisfaction.
Related resource: Additional evidence to quantify the value of flipped discharge
- Hospital at home (p. 27): Provide comprehensive, inpatient-level care in patients’ homes to avoid hospital stays altogether.
Related resource: Additional evidence to quantify the value of hospital at home
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.