Auto logout in seconds.
Continue LogoutAs AI becomes more prominent in healthcare, hospitals and health systems are racing to implement it across their operations. But while organizations have strategies to adopt and assess new technology, AI has created new challenges, making it harder to easily measure and show the value of these tools.
The healthcare industry leans in on AI
AI is a key focus for healthcare industry stakeholders, with many organizations having unveiled new AI tools, programs, and partnerships in recent months.
At the 2025 HLTH conference, which took place last month, several organizations highlighted their current AI efforts.
Currently, Endeavor Health is using Abridge's generative AI documentation tool and is piloting a nursing AI tool from Artisight. Similarly, Houston Methodist has implemented an AI-backed command center to coordinate and centralize care.
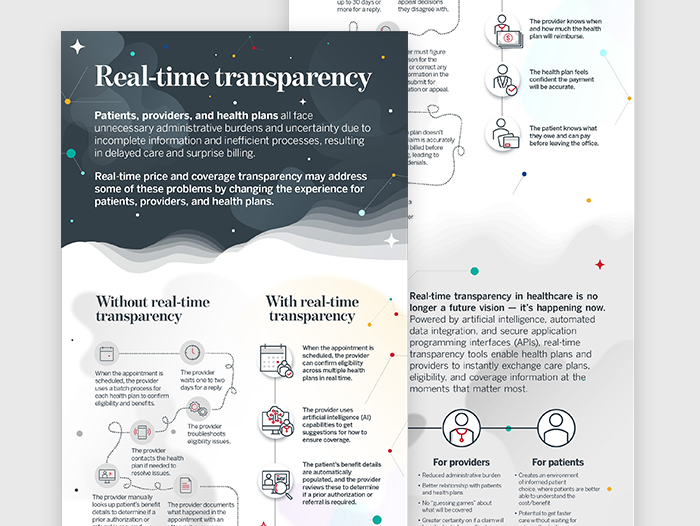
Optum* also announced a new AI-powered claims processing platform called Optum Real. The platform will connect payers' core systems and providers' EHRs to share and receive real-time information on claims-related queries, including prior authorizations, denials, and benefits coverage.
"AI technology really has taken us to the next level, or at least given us vision of what that next level is—to get as real time as possible," said Dave Ingham, chief information officer at Allina Health, which is currently piloting Optum Real.
How can health systems measure the value of AI tools?
Although many hospitals and health systems are investing heavily in AI, it's not always clear how to measure the technology's value.
"AI brings a set of new challenges since the pace of adoption is faster, and many of the performance indicators used historically will no longer be relevant or sufficient," said Carol Chouinard, VP and provider technology practice lead at Optum Advisory*.
For example, the benefits assessment for ambient AI listening tools would require organizations to combine several different metrics (patient experience, provider productivity for coding and documenting, quality of care, etc.) into one program — something that historically has not been done.
It can also be difficult to evaluate the financial impact of AI tools.
"In healthcare, particularly in the healthcare delivery side, it's really hard to apply line of sight to what we might think of as ROI," said Micky Tripathi, chief AI implementation officer at a major health system. "I don't think that any of us should really expect you're going to see a cost reduction that a CFO could look at and say, 'Oh, I see it there."
"AI brings a set of new challenges since the pace of adoption is faster, and many of the performance indicators used historically will no longer be relevant or sufficient."
To implement AI successfully, experts say that organizations need to think critically about the top problems they want to solve and their main priorities with AI tools. Organizations should also have a plan to evaluate AI tools, which can help determine if projects were successful financially or by other metrics.
"To me, step zero is being very, very clear about, what is it that we're doing? Why are we doing it? And what does success look like for that?" said Mouneer Odeh, chief data and AI officer at Cedars-Sinai.
Aside from measuring the financial impact of AI tools, organizations could also evaluate their impact on productivity, clinician burnout, and more.
According to Nele Jessel, CMO at health technology firm and EHR vendor Athenahealth, AI scribes can help providers complete notes more quickly and potentially see more patients. Providers may also be able to document services more accurately and bill for a higher level of services.
AI scribes could also help reduce clinician burnout and turnover by reducing the amount of time and effort spent on documenting care and other work in EHRs. This could lead to significant cost savings for hospitals and health systems since research suggests that replacing a physician can cost two to three times more than a physician's annual salary.
Advisory Board's AI resources
Patient satisfaction could also be an important metric for health systems to measure. Ambient AI scribes can help doctors be more present during appointments, and documentation assistants can help patients understand their care plans better.
"Providers are getting much better, for example, [at] vocalizing the physical exam, talking about the plan, right?" Jessel said. "So it increases the transparency and also makes it a much more enjoyable experience for patients."
However, if an AI tool only breaks even, organizations will need to determine if there are significant costs associated with it, like implementation expenses or using clinicians' time that could have been spent elsewhere. Unless the tool provides value in other areas, like freeing up clinician time so they can focus on patient care and use their full training and expertise, it may not be worthwhile.
"If you get to a place where you're just like, 'Hey, this thing didn't even break even. It doesn't even pay for itself.' Unless it's doing something absolutely miraculous for patients, it's out," said Anika Gardenhire, chief digital and transformation officer at Ardent Health.
*Advisory Board is a subsidiary of Optum. All Advisory Board research, expert perspectives, and recommendations remain independent.
(Olsen, Healthcare Dive, 10/27)
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.