Auto logout in seconds.
Continue LogoutAnthem last week said it has updated its coverage policies for ED visits, following criticism of the insurer's policy to deny coverage of ED visits for minor conditions that could "safely [be] treated in less acute facilities."
Learn more: Get the primers for reducing avoidable ED utilization
Background
Jay Moore, CMO for Anthem Blue Cross Blue Shield (BCBS) Missouri, said Anthem's policy has long been part of coverage contracts, although it has not always been enforced. The insurer decided to begin enforcing the policy, Moore said, to stem increasing costs related to inappropriate ED use.
According to Modern Healthcare, Anthem has been enforcing the policy in Georgia, Indiana, Kentucky, Missouri, New Hampshire, and Ohio. In its notifications, Anthem urged members dealing with non-emergency conditions to seek out medical help at urgent care facilities or retail clinics, or to contact Anthem's telehealth services and 24/7 nurse hotline.
The ED policy does not apply if:
- The member is 13 years old or younger;
- The member was directed to the ED by a physician;
- An urgent care center is not within 15 miles of the member; and/or
- The visit occurs over the weekend or on a major holiday.
However, providers and patient advocates pushed back against the policy, saying it could discourage members from getting needed care. For instance, Jonathan Heidt, president of the Missouri chapter of the American College of Emergency Physicians (ACEP), said his hospital "was receiving denials within days" of the policy taking effect.
Anthem adds exceptions to policy
Anthem last week said it has added several new exceptions to its ED policy effective Jan. 1. Under the expanded exceptions, Anthem said the ED policy will not apply if the member:
- Is directed by a health care provider to visit the ED;
- Is traveling out of state;
- Is younger than 15; and
- Received surgery, IV fluids, IV medications, an MRI, or a CT scan during his or her ED visit.
Anthem said it will apply the exceptions to previously denied claims and will request medical records from hospitals when it reviews ED claims. The insurer in a statement added, "We will continue to review this list and may expand it."
Comments
Anthem said while it will change the avoidable ED program to ensure affordable and appropriate care, EDs remain a costly location to treat routine health problems. "Anthem's avoidable [ED] program aims to reduce the trend in recent years of inappropriate use of [EDs] for non-emergencies," the insurer said. "We recognize, however, that there are ways to further improve and enhance the program."
However, some providers and lawmakers say the changes do not go far enough, Modern Healthcare reports. ACEP President Paul Kivela said the expanded exceptions "do not address the underlying problem of putting patients in a potentially dangerous position of having to decide whether their symptoms are medical emergencies or not before they seek emergency care, or pay the entire bill if it's not an emergency."
Separately, Sen. Claire McCaskill (D-Mo.), who is examining the policy to see if it violates any laws, also said the policy continues to put "the onus on someone who has no medical training to determine whether or not they should go to the [ED]" (Livingston, Modern Healthcare, 2/15; Baker, "Vitals," Axios, 2/16; Morse, Healthcare Finance News, 2/19).
Next, get primers for reducing avoidable ED utilization
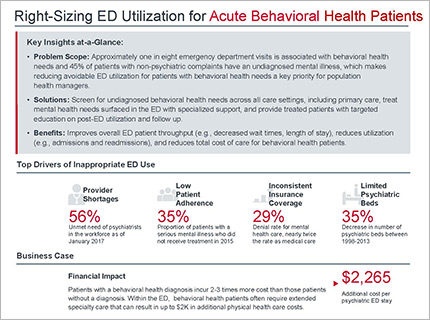
Are specific patient populations making up a significant proportion of your ED visits? Each installment in our Right-Sizing ED Use primer series takes a lens to one of these frequent user subgroups.
We analyze the reasons these patients seek care in the ED, the business case for intervening, and solutions for reducing unnecessary ED use. The primers also feature in-depth case studies which highlight the operational details of successful and targeted programs from leading health care organizations.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.