Auto logout in seconds.
Continue LogoutBy Ethan Brosowsky and Scott Orwig
Health systems have long been engaged in a delicate cost-control dance: Given the importance of maintaining relationships with physicians, many organizations have attempted to pursue cost-cutting strategies that do not affect doctors, out of a fear of jeopardizing referrals and related revenue.
But a hands-off strategy is untenable in today's health care environment, in which margins are often razor-thin, risk-based policies increasingly reward care management over high-revenue procedures, and more doctors are directly employed by hospitals and health systems.
Keep reading to two keys for partnering with physicians to rein in costs.
Then, join us on Friday, Jan. 12 for Part 1 of our webconference series on the high-performing clinical enterprise, when our experts will take a deep-dive into how to partner with physicians on your enterprise cost control strategy.
Understand the urgency—and the opportunity
Most hospitals and health systems' cost structures aren't just problematic—they're unsustainable. In fact, a 2016 Congressional Budget Office analysis of 3,000 hospitals found that if the organizations didn't increase productivity or otherwise reduce cost growth, 60% of them would have negative profit margins in 2025, with an average profit margin across all hospitals of negative 0.2%.
No matter the payment model, controlling enterprise costs—that is, costs driven by labor and facilities—is the ultimate no-regrets solution to today's unsustainable margins. So where do physicians come in to play? Here are the two primary ways in which physicians impact the cost of care delivery:
Non-labor costs: Even conservative Advisory Board estimates indicate that a 350-bed hospital in the highest performing quartile could save a minimum of 16% in total direct costs for Medicare fee-for-service cases by reducing variation in non-labor costs, including in supplies, ICU/CCU utilization, length-of-stay, and lab tests and imaging.
Labor costs: These are the costs of building and maintaining the system's physician enterprise and are determined by the size of the network, the use of physician employment, the level of compensation, and provider burnout and turnover. There are huge costs associated with running a physician enterprise—especially an employed one. On average, a health system invests about $65 million in its employed medical group annually.
Follow the 4 steps to enable cost-conscious care delivery
Reducing clinical care variation has long been a priority for hospitals and health systems—but achieving it is easier said than done. To get started, organizations need to ask themselves four questions:
1. What is the cost opportunity and where do we start?
2. How do we design and scale standards across the enterprise?
3. How do we implement standards into clinical practice that make adherence the default option?
4. How do we motivate physicians to develop and adopt new care standards?
One organization that has successfully engaged—and empowered—physicians to reduce unnecessary care variation is Carolinas HealthCare System, a 41-hospital health system based in Charlotte, North Carolina.
After a decade of establishing a system-wide quality infrastructure, system leaders began to engage physicians in conversations about cost of care and established a clinical optimization initiative. Previous system-led attempts to control costs had failed to secure physician buy-in, so it was clear a new system was necessary.
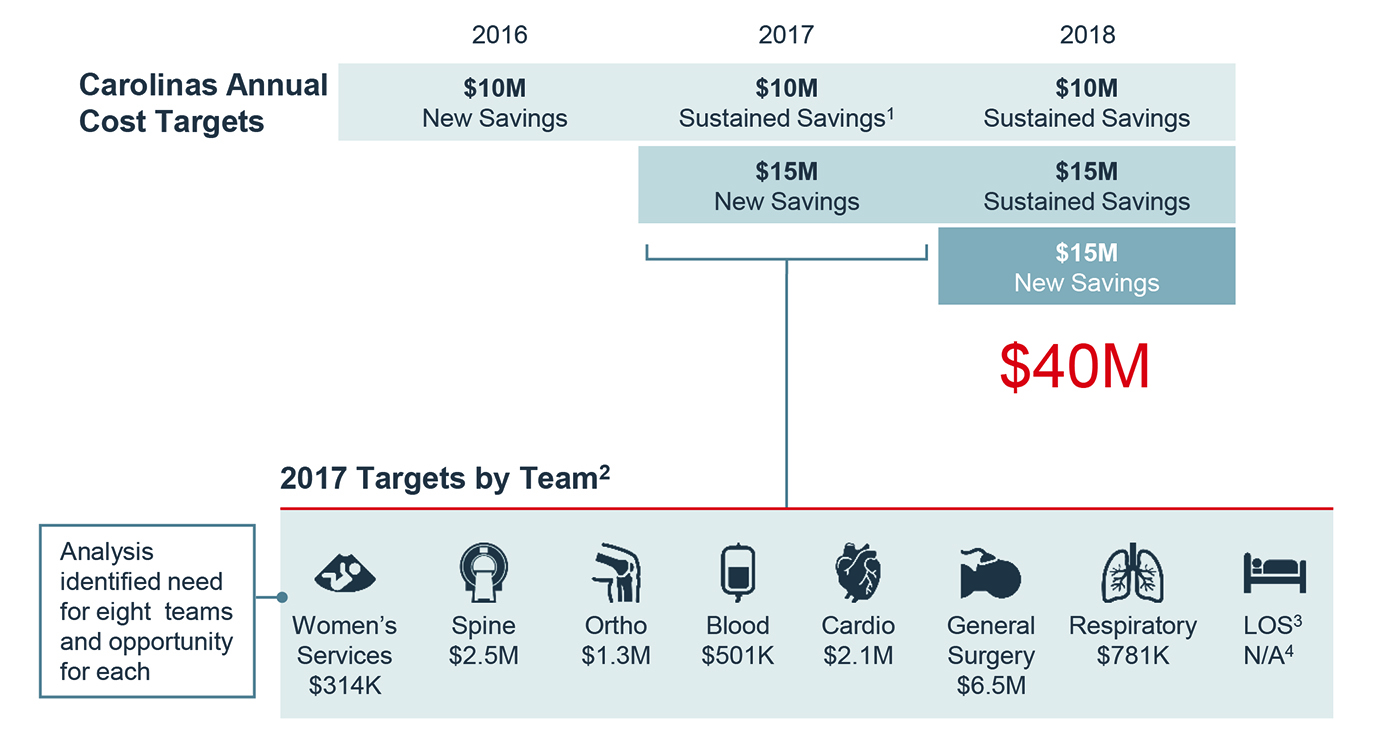
Carolinas first benchmarked its quality and cost data against peer institutions, then determined
areas where the system was an outlier by comparing their average cost per case to the cohort. Using this information, Carolinas compared cost and quality variation across facilities to estimate the potential savings of each facility performing like their best in-system peer, then set targets for physician-led clinical optimization teams at each facility. Ultimately, the system arrived at a $40 million clinical optimization goal across four years and created eight different groups across service areas to seize the opportunities.
During conversations with Advisory Board researchers, physicians involved with the clinical optimization efforts said that having the autonomy to set their own strategy to achieve their savings target was critical, and that it allowed them to effectively partner with their peers to find the best opportunities to reduce variation and cut costs. Rather than simply issuing a top-down mandate, physicians were given autonomy to approach cost-cutting as if they were running their own practice.
As of 2016, Carolinas had achieved over $26 million in variable cost savings and the plan's popularity with physicians led to additional service lines requesting their own clinical optimization teams.
Next, join our webconferences to learn more
Our two-part webconference series offers seven practices that bring margin management to the forefront of system-physician relationships. Join us for Part 1 on Friday, Jan. 12 to learn how to partner with physicians in enterprise cost control.
Register Now
Then, join us for Part 2 on Friday, Jan. 26 to learn how to design the efficient clinical enterprise.
Register Now
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
