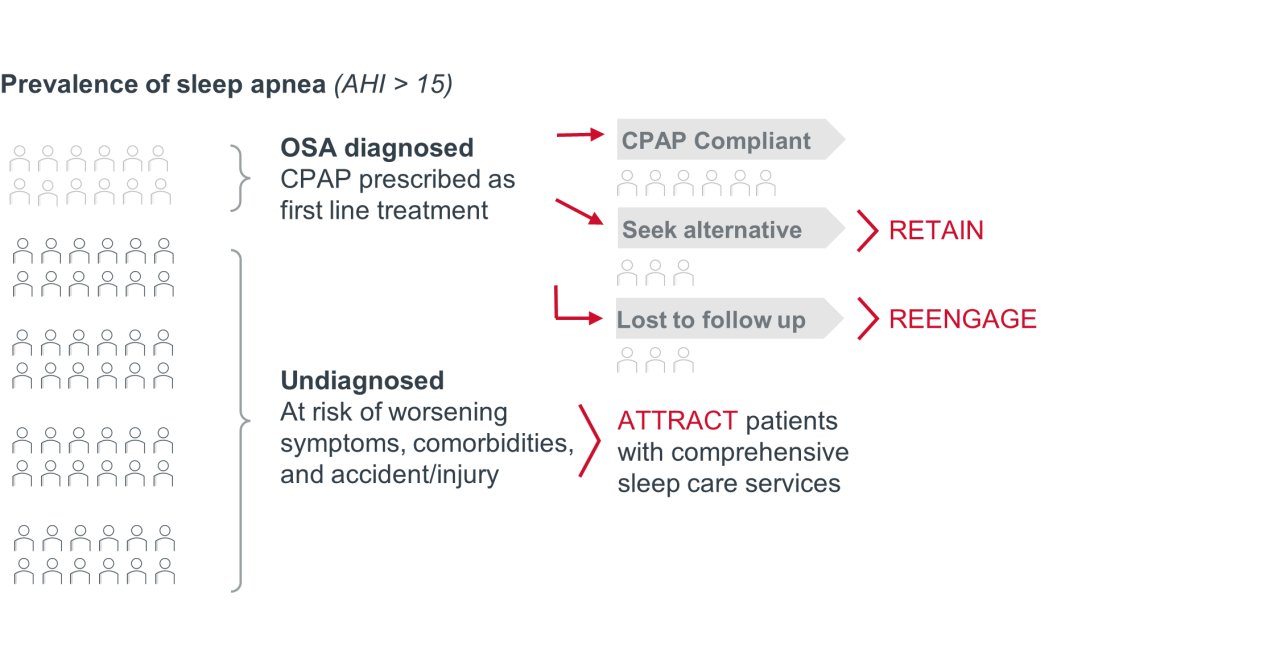
Sleep apnea is a disorder characterized by pauses in breathing during sleep, due to a partially or completely obstructed airway. There are two main types of sleep apnea: central sleep apnea (CSA), which occurs when the brain does not send the proper signals to the muscles to control breathing, and obstructive sleep apnea (OSA), which occurs when the airway becomes blocked during sleep. While OSA ranks as the second most prevalent sleep disorder globally, following insomnia, it remains significantly underdiagnosed. Of an estimated 30 million people in the United States living with OSA symptoms, only about 20% or 6 million people are diagnosed.
3 reasons to prioritize comprehensive sleep services
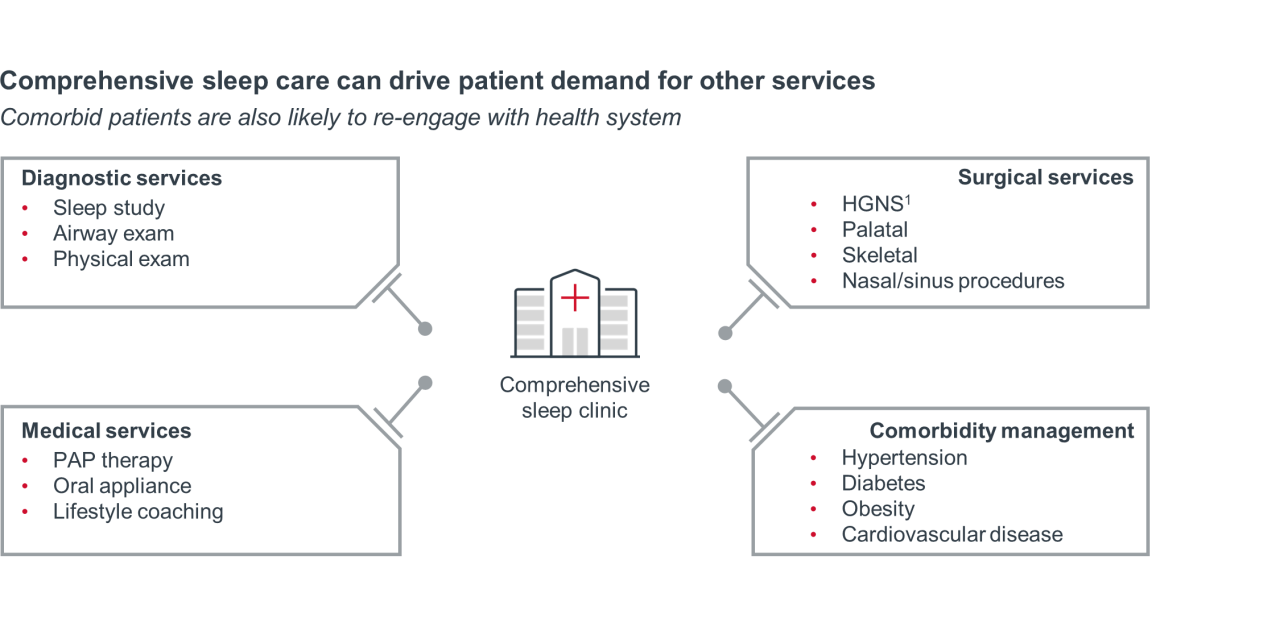
OSA has significant economic and population health implications. Untreated OSA raises the risk of comorbidities like cardiovascular disease, diabetes, depression, and accidents due to daytime sleepiness. Underdiagnosing sleep disorders leads to increased healthcare utilization, resulting in an increase in healthcare expenditures of nearly $7,000 per undiagnosed patient per year. Patients who receive a diagnosis are typically prescribed continuous positive airway pressure (CPAP) therapy as the primary treatment for OSA. However, many patients face difficulty adhering to CPAP, leading to undertreatment. The health care costs of underdiagnosing and undertreating sleep apnea are estimated at $94.9B annually. The upfront costs associated with treating sleep disorders may be high depending on treatment type, but comprehensive treatment options can generate significant cost-savings by improving outcomes, reducing long term health risks and utilization, and creating a competitive advantage for care delivery organizations.
The future of the sleep care services market
The sleep apnea device market is valued at $9.6B in 2023 and expected to grow to $17B by 2032, driven by the increasing incidence of sleep apnea, its comorbidities, and technological advancements. Comprehensive sleep services centered on proper diagnosis and tailored treatment for OSA are economically crucial for care delivery organizations. However, limited awareness among providers and patients, limited capacity, and inadequate care coordination pose challenges to market growth and hinder the provision of comprehensive sleep care. Collaboration across multiple sites of care — sleep clinics, ambulatory surgical centers, hospitals, and health systems, as well as different medical specialties — is key to attracting, retaining, and reengaging patients in need of sleep apnea care.
"Prior to Inspire, patients would find their way into our office for other surgical attempts at treating their sleep apnea. But most of them were just continuing to suffer along and left their CPAP sitting in the closet."
Why is this a priority?
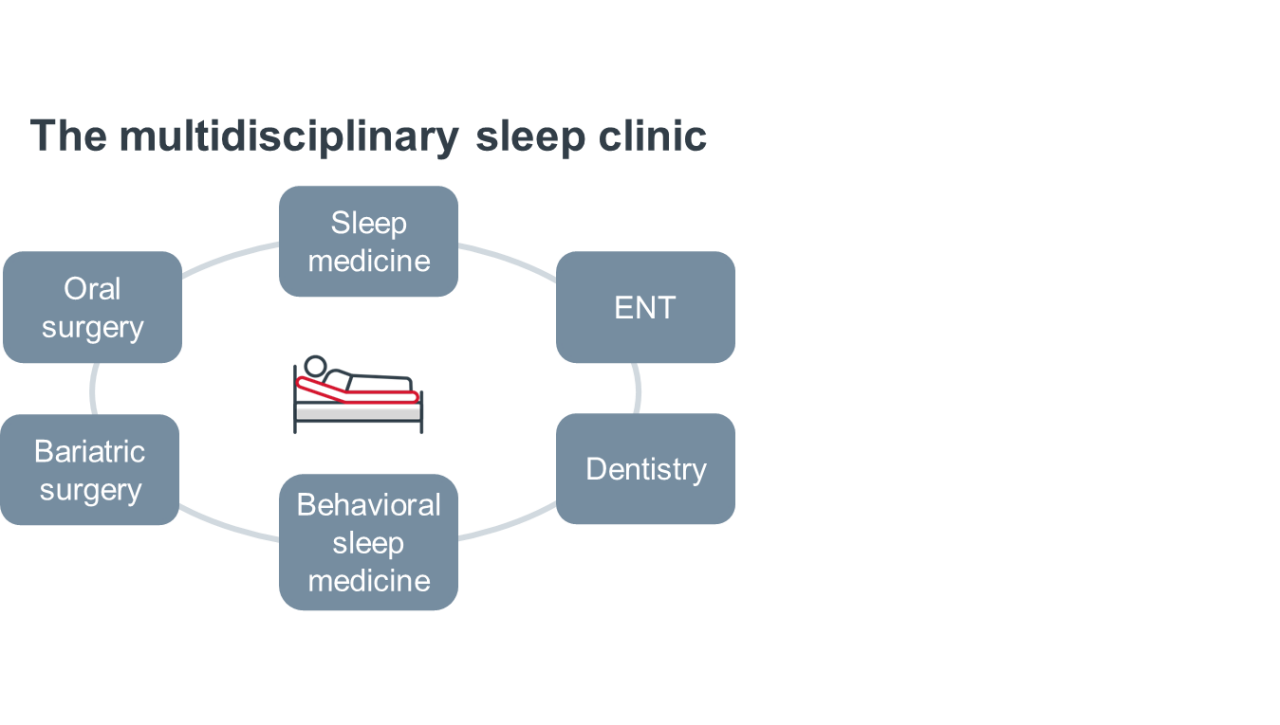
Obstructive sleep apnea diagnosis and treatment is complex and may involve a wide range of providers beyond sleep medicine specialists, including pulmonologists, otolaryngologists, neurologists, and dentists. OSA treatments — such as continuous positive airway pressure (CPAP) or hypoglossal nerve stimulation (HGNS) — require multidisciplinary collaboration, comprehensive care coordination, and long-term management. However, limited specialist capacity and a lack of capacity among primary care providers (PCPs) creates challenges for both doctors and patients.
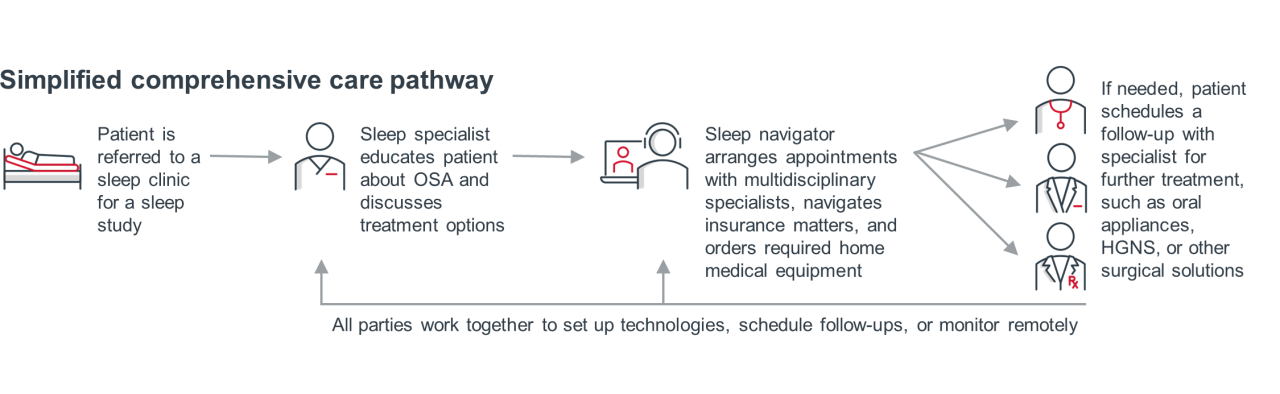
Connecting patients to the right providers at the right time is thus essential to treatment success. Familiarity with OSA is crucial for PCPs, because they are often patients’ first point of contact before referral to a sleep specialist. Similarly, specialists in diseases that are highly comorbid with OSA — particularly cardiologists — can be key to identifying undiagnosed OSA patients. Collaborating with sleep specialists can help PCPs and other specialists better screen for OSA, become familiar with treatment options, and clarify patient pathways. For example, innovative screening tools, such as EMR screening driven by predictive AI, can improve providers’ ability to recognize when to refer to a sleep specialist.
Sleep care navigators help patients stay connected to the OSA management process once they enter the sleep pathway by scheduling follow-ups with other specialists, setting up and monitoring home medical equipment, and making sure providers are communicating with each other. This kind of comprehensive care coordination ensures that patients can access convenient screening, treatment, and follow-up services — and helps healthcare organizations realize the business development opportunities and cost savings of properly treating OSA.
What do healthcare executives need to know?
- Effective care coordination and patient engagement increase the likelihood of adherence to prescribed therapy, optimizing therapeutic outcomes for OSA patients.
- Sleep apnea management is most effective when it involves a collaborative, multidisciplinary team of PCPs, and specialists in sleep medicine, otolaryngology, pulmonology, or neurology.
- Successful integration of service lines requires communication and training among PCPs and specialists to provide optimal care coordination.
How should stakeholders strategize?
Clinical
- Develop standardized care pathways for sleep disorder patients that outline the roles and responsibilities of each healthcare provider involved, specifies communication channels, and establishes clear guidelines for referral and follow-up. Outline a step-by-step process for patient evaluation, diagnostic testing, treatment options, and follow-up care. Work across service lines to give PCPs and other specialists clarity about their role in the care pathway.
- Consider deploying advanced practice providers (APP) to expand the capacity of specialties to perform screening, diagnosis, and treatment services — enhancing timeliness of care and treatment success.
- Use virtual visits and remote monitoring technologies to stay connected to patients and monitor adherence to treatment, which will lead to improved patient outcomes.
Operational
- Add a sleep care navigator to ensure that OSA patients are properly diagnosed, scheduled for appropriate follow-up appointments, and educated about their disorder — boosting adherence, reducing overall costs, and increasing the likelihood of treatment success.
- Implement a centralized patient navigation system to guide OSA patients through the health system and coordinate appointments, tests, and treatments. This can include teaching patients about lifestyle modifications, proper use of equipment, and self-monitoring techniques, reducing the need for frequent clinic visits and improving patient outcomes.
- Analyze OSA care pathway data, including patient outcomes, length of stay, readmission rates, and patient satisfaction scores to identify and correct inefficiencies in the process.
Financial
- Maximize program value by establishing a referral coordination team consisting of registered nurses and medical support administrators to screen potential patients for OSA and obtain sign-off from a sleep specialist. Streamlining this process allows care delivery organizations to enhance care coordination, improve efficiency, and reduce costs.
Why is this a priority?
It is common for patients who receive an OSA diagnosis to have other comorbid conditions. In fact, a 2022 study found that 63% of individuals diagnosed with sleep apnea had at least one comorbid condition, including obesity, cardiac disorders, diabetes, mental health disorders, and insomnia. Often, sleep apnea and its comorbid conditions exacerbate one another, leading to an increased risk of cardiac events, high blood pressure, insulin resistance, and poor mental health. Although there have been few effective treatment options in the past, mass media education has increased both public awareness of the condition and new therapies for managing it. Prioritizing sleep care and offering a variety of targeted therapies like CPAP, oral appliances, surgery, and hypoglossal nerve stimulation can provide effective treatment options for OSA and reduce symptoms of comorbidities — decreasing healthcare utilization costs overall.
However, not all patients will adhere to the most common OSA therapy, CPAP. Health systems offering comprehensive sleep care will have an opportunity to strategically re-engage with CPAP non-adherent patients and patients who return to the health system to manage other conditions.
Of individuals diagnosed with sleep apnea had at least one comorbid condition
Common comorbid conditions among OSA patients
Obesity: In the U.S., obesity currently affects 4 out of 10 Americans. Studies have shown obesity can make OSA worse by diminishing airflow: An increased amount of fat in the neck may block the airway, and excess abdominal girth can compress the chest wall and decrease lung volume. OSA can also make it difficult to lose weight, as poor sleep quality can lead to increased appetite. Although weight management alone is not a cure-all for OSA, it may be an essential first step in reducing and managing symptoms.
Cardiac disorders: There is a strong association between patients with OSA and cardiac issues, including cardiovascular disease (CVD), atrial fibrillation (AF) and other cardiac arrythmias, heart failure, pulmonary hypertension, and stroke. Not only are patients with CVD 40%-80% more likely to have OSA, but the risk for atrial fibrillation is 2-4x higher among OSA patients, and middle-aged men with severe OSA are 58% more likely to develop heart failure. However, properly treating sleep apnea lowers the risk of OSA symptoms exacerbating cardiovascular illness: A recent study found that if patients adhere to CPAP therapy for at least 4 hours a night, there is a reduced recurrent risk of major adverse cardiac or cerebrovascular events. Another study concluded CPAP therapy leads to a reduction of recurrent AF by 56%.
Diabetes: The American Diabetes Association estimates that up to one in four people with type 2 diabetes also has OSA. Because OSA is associated with insulin resistance and changes in glucose metabolism and can lead to elevated A1C, high blood pressure and heart problems, diabetes management becomes challenging when OSA is left untreated. Fortunately, OSA treatment has been found to improve blood sugar control in patients with diabetes: A recent study found that 59% of diabetic patients improved their blood sugar control when adhering to CPAP. While CPAP therapy may not “cure” diabetes, it can reverse certain symptoms and improve blood sugar control.
People with type 2 diabetes also have OSA
Insomnia: Comorbid insomnia and sleep apnea (COMISA) is another a common sleep disorder. A person with either OSA or insomnia has a 30%-50% chance of having the other, likely because obstructed breathing can cause frequent arousal from sleep and difficulty falling or staying asleep. Research suggests that these two diseases combined carry a higher risk of mortality: COMISA participants had a 47% increased risk of all-cause mortality compared to participants without insomnia or sleep apnea. But although insomnia and OSA are separate disorders, it is possible to treat both simultaneously through a combination of therapies, including, but not limited to, interventions to keep the airway open during sleep, medication, and cognitive-behavioral therapy.
Mental health: Sleep problems are both a common symptom and a cause of many mental health disorders. A study evaluating the prevalence of mental illness in OSA patients found that of 182 patients who underwent polysomnography, 46.7% also presented with a psychiatric disorder, most commonly depression and anxiety. Timely screening and diagnosis for mental health disorders among OSA patients can facilitate better interventions and improve patients’ quality of life.
What do healthcare executives need to know?
- In the U.S., approximately 24 million individuals suffer with an undiagnosed sleep disorder and the number of people with comorbid conditions is increasing. By offering comprehensive sleep services, care delivery organizations can attract and strategically re-engage these patients.
- The demand for sleep services is increasing, patients are becoming more aware of CPAP alternatives like HGNS/Inspire therapy — approximately 12 million web users visited the Inspire website in 2023.
- Because at least 50% of individuals discontinue the usage of CPAP therapy after one year, there is a growing need for alternative and combination therapies.
- There is an urgent need for increased provider and patient education about common sleep disorders and routine screening services. Primary care physicians and specialists treating common comorbidities, such as cardiology and endocrinology, have a unique opportunity to improve population health and access through OSA screening, identification, and referral of patients with suspected sleep apnea.
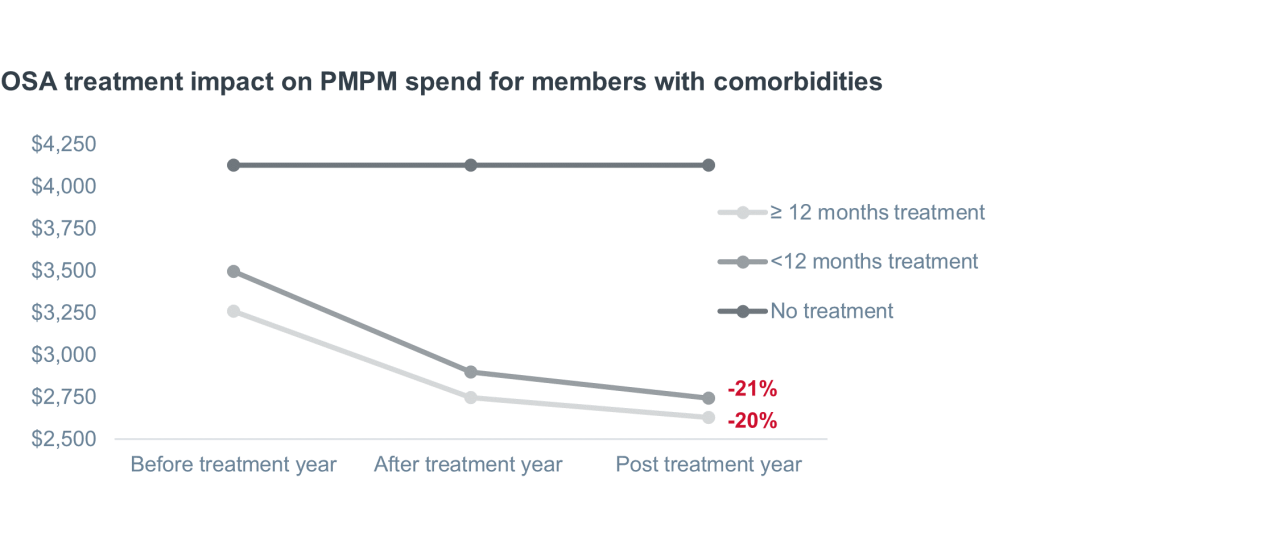
- Addressing sleep apnea at the population level can reduce spend as Medicare beneficiaries with comorbidities saw a 20% and 21% per member per month (PMPM) spend reduction within a year or more of OSA treatment.
How should stakeholders strategize?
Clinical
- Offer convenient and accessible diagnostic testing options, such as home sleep apnea tests, which can increase patient participation and early detection.
- Adopt a comprehensive, patient-centered approach to sleep apnea and its comorbidities by optimizing care team models across specialties — such as cardiology, pulmonology, endocrinology, otolaryngology, psychiatry, bariatrics, and sleep medicine — to ensure patients receive timely access to care with appropriate providers. Leverage APPs when necessary.
- Holistically treat sleep apnea patients by providing counseling services to help patients manage stress and anxiety and behavioral intervention to support lifestyle changes — increasing patient satisfaction and the likelihood of those patients being returning customers.
Operational
- Strengthen care coordination between sleep clinics, hospitals, ambulatory surgical centers (ASCs) and referring physicians by prioritizing frequent communication between care centers and sharing patient information to establish seamless referral pathways.
- Build out partnerships with referring physicians and healthcare organizations by making in-person connections and emphasizing the financial and clinical benefits of comprehensive sleep care.
- Provide education and awareness programs to primary care physicians and the community to promote the importance of sleep health and encourage referrals to the clinic.
- Market sleep care services to potential patients by advertising through digital channels, such as social media and email campaigns.
Financial
- Collaborate with payers and insurers to advocate for policy coverage or expand coverage options for sleep disorder treatment to help reduce financial barriers for patients seeking care.
- Consider investing in a physician liaison to help educate and collaborate with PCPs so they are aware of sleep services available within the hospital, further increasing the likelihood of patient referrals for sleep services and avoiding patient leakage.
Higher PMPM spend among OSA patients vs. patients without OSA
Why is this a priority?
The sleep apnea treatment landscape is nuanced, and treatment options vary depending on disease severity, the type of sleep apnea, and other contributing factors. Therapies may include lifestyle changes, CPAP therapy, surgery, or a combination of the three. Although CPAP is the frontline treatment for moderate to severe OSA, many patients have difficulty sticking with it. Studies indicate that adherence rates for CPAP therapy are as low as 54%, with some studies showing even lower rates of adherence.
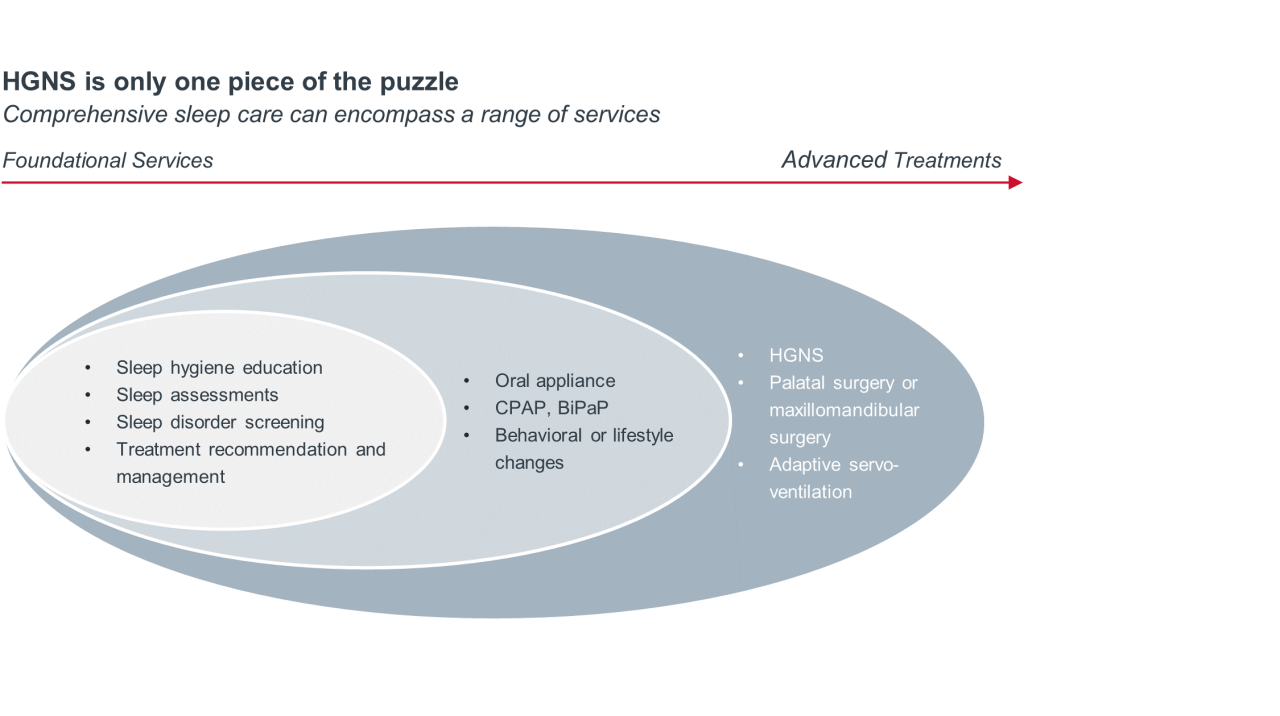
Nonadherence to CPAP treatment leads to worse outcomes and increases 30-day all-cause and cardiovascular-related readmissions. With high early adherence rates (92.4% used the device consistently on most nights), hypoglossal nerve stimulation (HGNS) has been shown to be a successful alternative for CPAP-intolerant patients. In addition, a 2021 study showed sustained improvements in patient-reported outcomes after one year with HGNS. These positive outcomes have come with surprisingly few drawbacks. HGNS has a lower complication rate compared to multi-level surgery, 3% vs 22% respectively. When compared to palatal surgery, the complication rate lowers further to 2% vs.21% respectively.
In June 2023, the FDA expanded indications for HGNS, changing the upper BMI labeling warning for eligibility from 32 to 40 and increasing the baseline AHI range to 15-100 (from 15-65). These expanded patient criteria makes HGNS easier for patients to access — and care delivery organizations have an opportunity to facilitate that access. Convenient access to timely treatment makes OSA patients more likely to understand the severity of their disease and the importance of ongoing management, which may increase adherence to treatment and reduce costs long-term. To illustrate, in a study of Medicare patients with co-morbid cardiovascular disease, OSA patients who successfully adhered to treatment lowered healthcare costs by 40%. Emphasizing early diagnosis and treatment options best suited to each patient can alleviate the increased care costs associated with untreated OSA.
What do healthcare executives need to know?
- Coding, coverage, and payment for HGNS therapy are well established for both Medicare and private insurance (see Table 1, Table 2). However, the HGNS treatment landscape is evolving, so it is important to stay up-to-date on regulatory changes.
- HGNS therapy is an AASM1-certified treatment to meet quality measures for OSA and offers a viable alternative for patient who cannot tolerate CPAP therapy.
- Developing protocols to assess patient eligibility and facilitate referral for HGNS is essential.
Physician reimbursement schedule2
| Service | Description | CPT code | Payment | Work RVU4 |
| Initial consultation | Straightforward MDM3 or 15-29 minutes | 99202 | $72.86 | 0.93 |
| Low level MDM or 30-44 minutes | 99203 | $112.84 | 1.60 | |
| Moderate level MDM or 45-59 minutes | 99204 | $167.40 | 2.60 | |
| High level MDM or 60-74 minutes | 99205 | $220.95 | 3.50 | |
| Qualifying sleep tests | Polysomnography (PSG) | 95810 | $615.05 | 2.50 |
| Home sleep test (HST) | 95800 | $150.80 | 0.85 | |
| Follow-up consultation | Presenting problems are minimal | 99211 | $23.38 | 0.18 |
| Straightforward MDM or 10-19 minutes | 99212 | $56.93 | 0.70 | |
| Low level MDM or 20-29 minutes | 99213 | $90.82 | 1.30 | |
| Moderate level MDM or 30-39 minutes | 99214 | $128.43 | 1.92 | |
| High level MDM or 40-54 minutes | 99215 | $179.94 | 2.80 | |
| HGNS procedure | Drug-induced Sleep Endoscopy (DISE) | 42975 | $96.92 | 1.58 |
| Inspire implant | 64582 | $872.60 | 14.00 |
Facility reimbursement changes
| Facility | Description | CPT code | 2023 payment | 2024 payment |
| Hospital outpatient | Hypoglossal nerve stimulation (HGNS) | 64582 | $29,358 | $29,617 |
| Drug-induced Sleep Endoscopy (DISE) | 42975 | $179 | $1,619 | |
| Ambulatory surgical center | HGNS | 64582 | $25,180 | $24,870 |
| DISE | 42975 | $93 | $757 |
How should stakeholders strategize?
Clinical
- Attract patients who are actively searching for sleep apnea treatment options with digital marketing campaigns that increase awareness about the benefits of HGNS therapy for sleep apnea. Strategies like online advertisements and search engine marketing can reach potential patients looking for CPAP alternatives.
- Conduct outreach programs to educate local physicians about the availability and benefits of HGNS therapy. Leverage existing networks within the health system to expand access to sleep care services and ensure that patients have options for evaluation, treatment, and follow-up care.
- Collaborate with ASCs to offer HGNS therapy as an outpatient procedure, increasing its convenience and expanding accessibility for patients.
Operational
- Establish a streamlined referral and evaluation process by working with sleep medicine specialists, pulmonologists, and other healthcare providers to establish clear referral criteria that is easily understood by referring providers. Consider investing in a centralized referral management system or team to oversee the referral process for HGNS therapy and facilitate timely access.
- Create a dedicated sleep services line that offers multidisciplinary sleep care services, aligning sleep medicine specialists with PCPs, pulmonologists, and other relevant providers to develop referral networks and guide the patient pathway to facilitate access to HGNS therapy.
- Obtain accreditation and certification to perform HGNS procedures, and develop streamlined processes for patient scheduling, pre-operative assessments, and post-operative care to plan for the growing demand for HGNS procedures and optimize patient experience.
Financial
- Conduct cost analyses to identify areas for cost optimization and efficiency improvement in the delivery of HGNS therapy by evaluating supply chain management, resource utilization, and operational processes to reduce costs without compromising patient outcomes.
- Facilities should develop partnerships with insurance providers to negotiate favorable reimbursement rates and coverage for HGNS therapy by compiling evidence-based research, clinical outcomes, and patient success stories — demonstrating the efficacy and cost-effectiveness of HGNS.
"In this case, Inspire benefits both the GI and ENT surgical service lines, but most importantly the outcomes are good."
The future of sleep care services
The future of sleep services lies in embracing technological advancements like HGNS and implementing a collaborative approach to deliver comprehensive care to patients in need. The recent FDA expansion of indications for HGNS make it more accessible to a wider range of patients. Increasing reimbursement rates for facilities make the provision of HGNS more attractive to ASCs and hospitals. Stakeholder collaboration across sites of care is needed to meet rising patient demand for CPAP alternatives. Early diagnosis and tailored treatment options can effectively curb unnecessary healthcare costs associated with OSA and improve the quality of life for the millions of individuals who are undiagnosed or untreated.
1Hypoglossal nerve stimulation.
2American Academy of Sleep Medicine.
32023 Medicare National Average Physician Payment (Non-fac).
4Medical decision-making.
5Relative value units.
Inspire Medical Systems, Inc., is a medical innovation company committed to the safe, effective, and reliable treatment of obstructive sleep apnea in order to improve patient lives.
Inspire® therapy is a solution for people with obstructive sleep apnea who have tried and struggled with CPAP. The Inspire® implant works inside the body to treat the root cause of OSA, enabling patients to breathe regularly and sleep soundly. Learn more at inspiresleep.com.
This report is sponsored by Inspire, an Advisory Board member organization. Representatives of Inspire helped select the topics and issues addressed. Advisory Board experts wrote the report, maintained final editorial approval, and conducted the underlying research independently and objectively. Advisory Board does not endorse any company, organization, product or brand mentioned herein.
To learn more, view our editorial guidelines.

This report is sponsored by Inspire. Advisory Board experts maintained final editorial approval, and conducted the underlying research independently and objectively. Inspire had the opportunity to review the article.
Learn more at inspiresleep.com.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights




