Auto logout in seconds.
Continue LogoutPlans have long known that pregnant members are a vulnerable and expensive subpopulation, worthy of extra care management efforts—but the challenge lies in identifying them.
When high-risk pregnant members are not identified—and not enrolled in care management— they’re more likely to have NICU admissions, which are 4-6 times more expensive than regular deliveries.
What Makes Identification Hard
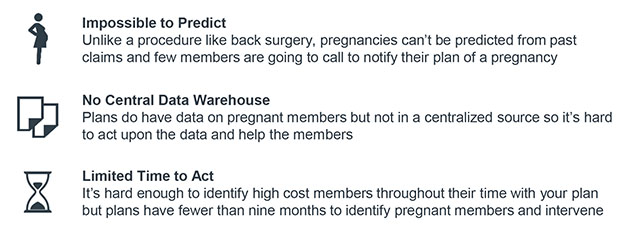
Even among high-risk members, there are three main reasons why early identification of pregnant members is especially difficult:
One Plan’s Solution
Health Partners Plan (HPP), a Medicaid plan based in Pennsylvania, recognized that they could identify more pregnant members by actively combining data sources and assigning care managers to conduct outreach. HPP’s data analytics team combines data from multiple sources into a single list of pregnant members, which then HPP’s care managers, named Baby Partners, use to conduct outreach and offer care management for high-risk members.
Results of the Baby Partners Program

Another Plan's Application
This year, Advisory Board hosted a cohort of plans that wanted to use lessons from HPP’s program to improve their own pregnancy care management programs. The cohort met via video conference every other month for six months. Health Plan of San Joaquin (HPSJ), a Medicaid plan based in California, took advantage of this cohort to revamp their pregnancy identification and stratification processes.
The plan collected data from various sources such as forms providers filled out, medical claims, and prescription data and used an algorithm to stratify the members by risk. They then focused outreach on the most vulnerable members:
- Members diagnosed as high-risk by a provider
- Members with an admission or ER visit in the last 90 days
- Members in the first and second trimester of pregnancy
- Members with social determinants of health concerns (especially homelessness)
Over the first six months, HPSJ increased their monthly number of identified high-risk pregnancies by 38% and even hired an additional case manager for their prenatal program to support the additional volumes.
Don't miss out on the latest Advisory Board insights
Create your free account to access 1 resource, including the latest research and webinars.
Want access without creating an account?
You have 1 free members-only resource remaining this month.
1 free members-only resources remaining
1 free members-only resources remaining
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
This content is available through your Curated Research partnership with Advisory Board. Click on ‘view this resource’ to read the full piece
Email ask@advisory.com to learn more
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.
Benefits Include:
This is for members only. Learn more.
Click on ‘Become a Member’ to learn about the benefits of a Full-Access partnership with Advisory Board
Never miss out on the latest innovative health care content tailored to you.


