Population health management is a collection of strategies that aims to improve the health of an entire population, using data to plan and deliver proactive care to maximise that population’s health and wellbeing.
Effective PHM focuses on the wider determinants of health, not just clinical care, and aims to improve health and wellbeing, prevent health deteriorations, and reduce inappropriate demand.
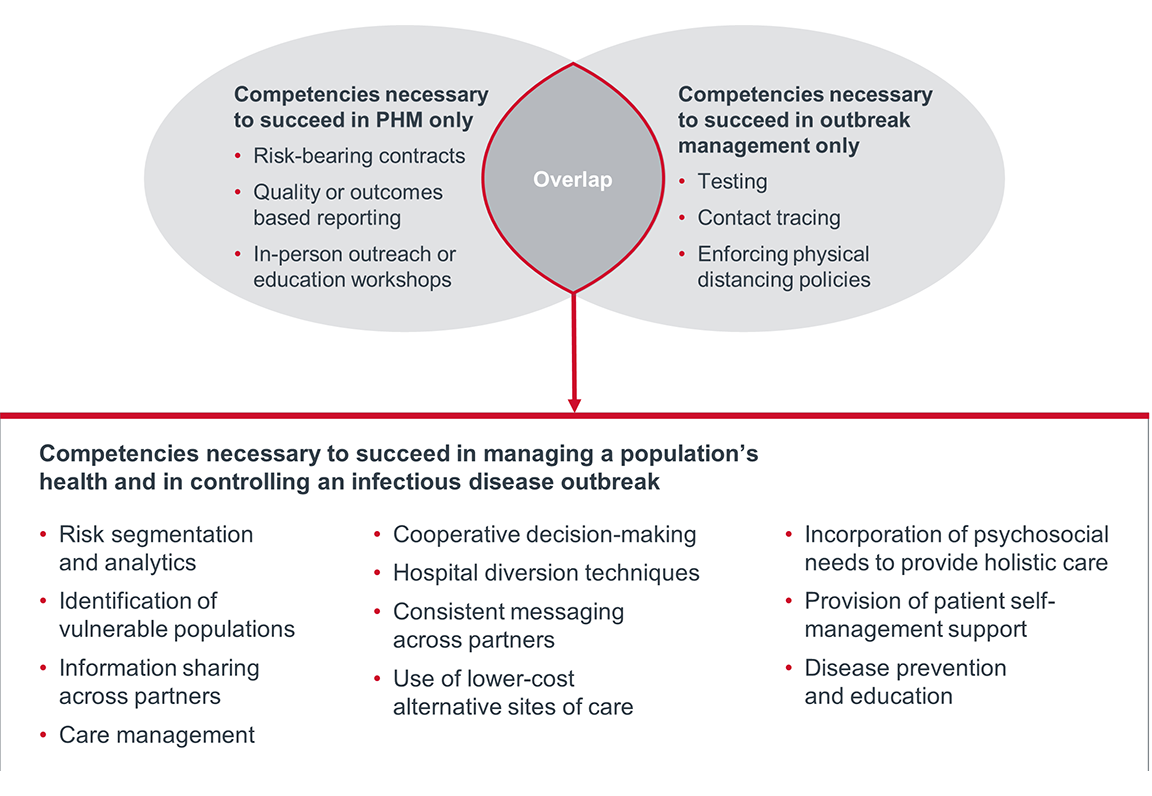
Effective population health managers typically build up a range of competencies and capabilities that enable this work. This includes:
- Cross-continuum data and analytics to understand population needs and inform resource allocation
- Robust partnerships or formal integration across the continuum, including with non-clinical organisations
- Services focused on proactivity and prevention
- Care models aimed at shifting care to lower-cost settings
- Payment models that incentivise proactive integrated care models
Over the past decade, many governments and providers have begun pursuing PHM to improve health outcomes and control health care spending.
Several root causes have driven this push towards PHM, such as ageing populations, growing rates of chronic disease, long wait times for care, and above all, increasing costs in health care.
Many clinical and political leaders view PHM as one of the top paths to achieve greater sustainability in health care and increase populations’ quality of life.
Many governments, including those of the United States, England, Ontario, Saudi Arabia, and Denmark, have introduced population health programmes. However, these government initiatives are often optional or phased over time, starting with initial cohorts of voluntary participants.
Even with government support, several barriers make PHM difficult to implement quickly: activity-based funding models; hospital-centric services; resistance to change; and legacy distrust between acute care and other providers.
As a result, progress at the organisational level has been varied despite national or local policy signals, which meant different institutions were at very different points in the journey towards PHM when Covid-19 hit in early 2020.
Organisations with robust PHM capabilities had faster, more coordinated, and more effective responses to the Covid-19 outbreak than those without. We predict that payers will more aggressively push towards PHM post-pandemic as affordability becomes the top issue for payers and publicly funded services in particular.
There’s significant overlap between the competencies necessary to succeed in managing a population’s health and in controlling an infectious disease outbreak.
The table below summarises how a few exemplar organisations used existing PHM competencies to enhance their responses to Covid-19.
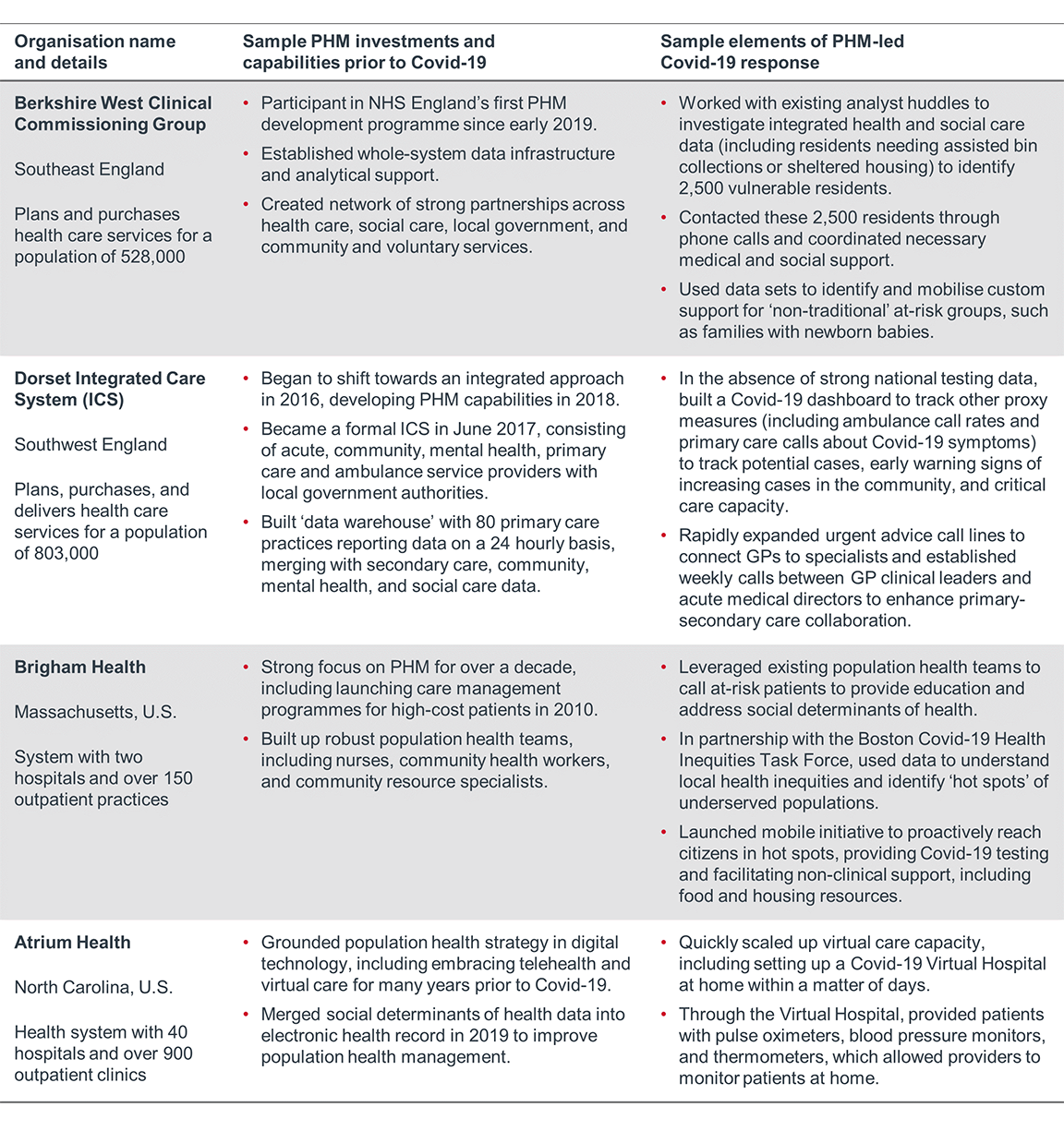
The foundations of PHM afford systems greater resilience by providing more flexibility to adapt and respond to new or more severe needs.
But the ‘stress test’ of Covid-19 revealed that the relationship between PHM investment and resilience is not proportional; that is, having started a little bit of the work here did not necessarily give systems a little bit more resilience. These competencies made a difference when they were mature and entrenched.
However, maturity isn’t the only element that makes for a successful population health manager. One great example of this is OhioHealth, a system with twelve hospitals and over 200 ambulatory sites in the U.S., which began focusing on population health management in early 2018.
In the face of Covid-19, OhioHealth delivered new telehealth access points, stood up home care services, and accelerated their analytics work. Their back-to-business plans focus on maintaining these improvements.
According to OhioHealth’s Senior Vice President of Population Health, “the pace of change and acceptance has definitely accelerated with the pandemic…the pandemic put [population health] front and center in a whole new way.”
As OhioHealth’s story demonstrates, ‘investment’ in PHM is not simply about time and money. It is also about the level of attention leaders put into shifting organisational culture and resources away from the status quo and towards a new vision.
If your organisation hasn’t already significantly invested in PHM, the Covid-19 crisis and restoration period present a unique opportunity to forge a PHM-oriented culture and accelerate the development of the PHM capabilities crucial for future success. On the following pages, we recommend what to do next.
Strong PHM competencies afforded systems greater resilience during the initial wave of Covid-19, and these competencies will be even more important going forward to meet payers’ demands to control costs while also improving populations’ wellbeing.
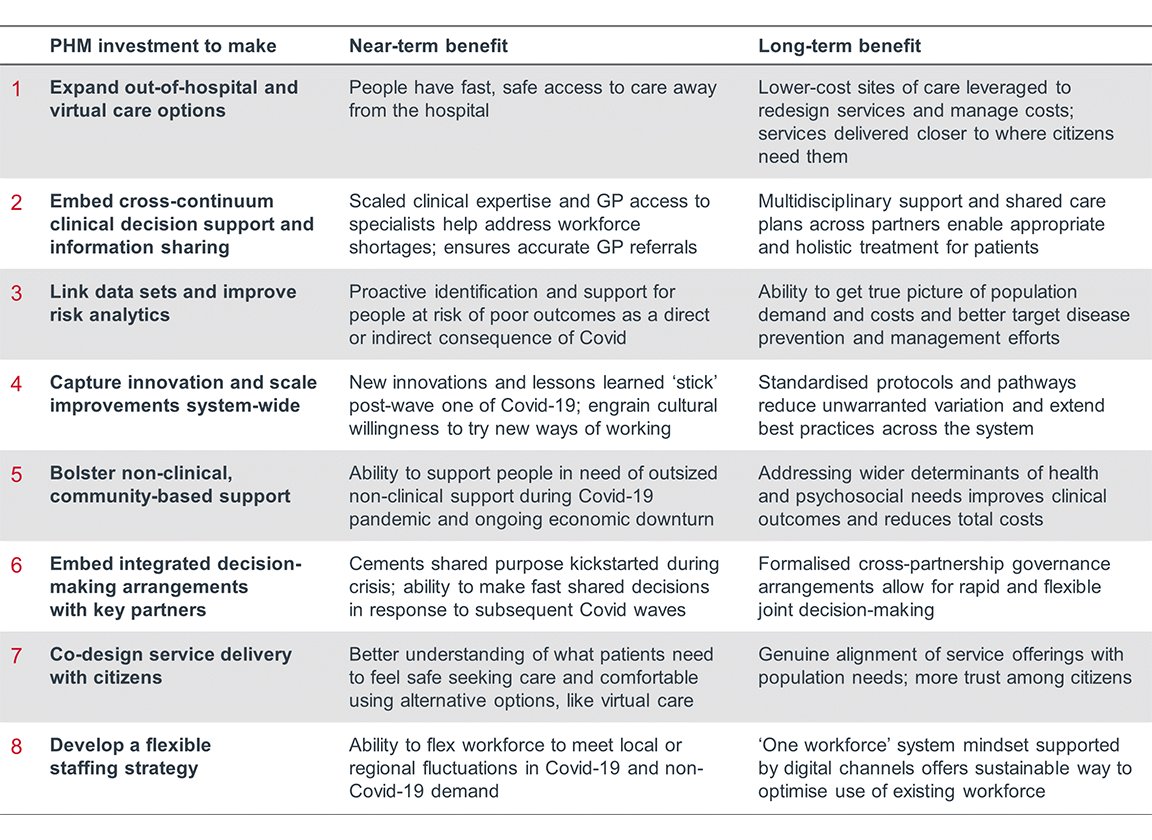
Covid-19 has created a unique window of opportunity to accelerate investment in PHM. Here’s what providers should do in the next three to twelve months.
Some jurisdictions, such as the NHS in England, are using Covid-19 as an opportunity to accelerate existing PHM and integration work. Many other governments are taking a step back from health care reform to give providers some breathing room to navigate the Covid-19 crisis and restoration period.
Regardless of whether it’s mandated or not, organisations must act now to accelerate investment in PHM capabilities. Covid-19 has lowered some of the barriers that have long prevented faster progress in PHM, giving systems a unique window of opportunity.
For example, Covid-19 forced a dramatic change in health care consumer habits away from the hospital, including towards telehealth. New ways of working led to new cross-continuum partnerships. And the crisis brought forward collective willpower to improve health care and an increased willingness to try new things.
Leaders should make use of the new habits formed during Covid and act while the memory of the pandemic is still fresh. The reduced obstacles—combined with the growing evidence of the value of PHM—provide a powerful opening for leaders to increase cultural commitment to PHM.
Systems that do this work now will have the added benefit of setting the pace in their markets, putting them in a unique position when regulators and policy makers pick this work back up. And since time is a key indicator of success in PHM, starting now will only provide an advantage in the long run.
Our research team has put together a list of the top eight PHM capabilities to bolster throughout Covid-19 response and restoration. We are seeing organisations start by prioritising up to three of these to ‘outperform’ on.
These specific capabilities can help in the near-term, to manage Covid and non-Covid demand, and in the longer term, to manage a population’s health.
Decades of research have proven just how strongly non-clinical factors influence health outcomes. Left unaddressed, non-clinical risk factors can drive avoidable utilisation and unnecessary spending.
Further, societal inequities perpetuate disparities in non-clinical risk factors, interfering with providers’ missions to help citizens live better and healthier lives.
In recent years, health care providers have begun to address the social determinants of health more thoroughly. But with competing priorities in the clinical world and outdated payment models, addressing non-clinical elements can feel out of reach, and so this work often doesn’t end up as a top priority.
However, Covid-19 has shone a spotlight on health equity, since it’s impossible to truly control and address the virus without accounting for non-clinical factors.
Across the world, the coronavirus hit low-income neighbourhoods and minority populations hardest. And in Singapore, mass outbreaks in overlooked migrants’ dormitories led to a second spike.
With historically underserved populations bearing the brunt of the pandemic, Covid-19 magnified what many already knew to be major cracks in the system.
If we’re going to succeed in containing Covid-19 (or other future pandemics), we must account for the social determinants of health and address health inequities. The same is true if we’re going to succeed long-term in managing the health of an entire population.
The first step in prioritising health equity in your organisational strategy is to clarify your ambition and role in relation to this work.
Below, we’ve outlined the primary roles for health care providers to become effective community partners and advance health equity. Determine which role(s) to play in partnership with community leaders who understand community needs.

Remember that the hospital should not independently own every PHM function— that is, the hospital should not always be the primary leader and decision-maker. Part of being an effective population health manager is rethinking who does what to ensure each system capability is led by the most appropriate stakeholder.
When we recommend investing in PHM competencies, sometimes this does mean hospital or health system leaders should build up capabilities internally.
Often, however, the acute sector is better suited to play a different role. Actively identify the best way for each partner to contribute to any given PHM initiative, and get comfortable with other partners taking on ownership.
For a hospital, the right role is often to amplify the work of other partners, which can take many forms—funding partners’ initiatives, sharing staff or administrative support, advocating for more resources, or getting the word out.
Before starting any PHM initiative, always stop to question if the hospital is truly the best owner. And for each capability, consider how the hospital should step up to lend support as well as how the hospital should step back to cede control.
Further, it’s likely that existing partners and even departments within your own organisation have the right expertise and have already begun building up some of these capabilities. Before starting from scratch, look for opportunities to learn and scale what’s working.
While there’s clearly a strong case for PHM capabilities during a pandemic, it’s likely they would help in the face of any shock to the health care system.
The foundations of PHM—data-driven action, a true understanding of population needs, genuine collaboration, streamlined decision-making—also afford systems greater resilience by providing more flexibility to adapt existing services to respond to new or more severe needs.
Further, these capabilities will be at even more of a premium going forward because the main drivers of PHM are still here—and in many cases are even stronger than they were pre-Covid.
Specifically, Covid-19 may exacerbate your population’s chronic conditions and behavioural health needs; quarantine may cause healthy people to deteriorate; the subsequent economic downturn may lead to worse health outcomes; and health care’s affordability problem will only be heightened as governments struggle to manage tighter budgets across all sectors.
In other words, Covid-19 hasn’t significantly changed the trajectory of health care: the same root cause problems remain, and PHM remains the most likely path forward.
Don't miss out on the latest Advisory Board insights
Create your free account to access 2 resources each month, including the latest research and webinars.
Want access without creating an account?
You have 2 free members-only resources remaining this month remaining this month.
1 free members-only resources remaining this month
1 free members-only resources remaining this month
You've reached your limit of free monthly insights
Become a member to access all of Advisory Board's resources, events, and experts
Never miss out on the latest innovative health care content tailored to you.
Benefits include:
You've reached your limit of free monthly insights


